|

Fever fits
Common condition in young children:
by Nilma DOLE
Parents should be cautious and mindful when their children have fever
fits because not all are related to epilepsy. More often than not, we
tend to worry about it confusing it with epileptic fits but for any
problem, a medical consultation is vital to determine what exactly is
the cause. President of the College of Paediatricians, Dr. Deepthi
Samarage spoke to the Sunday Observer about a particular type of
fainting attack called fever fits.
 Q:
What are febrile convulsions (fever fits) ? Q:
What are febrile convulsions (fever fits) ?
A: Febrile convulsions (also called fever fits, fits with
fever or febrile seizures) is a common condition in children, in the age
group of six months to about six years. They occur in 3-4% of all
children.
The child loses consciousness briefly and may develop jerky movements
coupled with a bout of fever.
This is not a prolonged fever because it is nothing to worry about
but parents should ensure that the child is safe and not in harm’s way.
Q: Do fever fits need prompt treatment if there are repeated
fits?
A: No. Since it is an age-related condition, it will pass when
the child becomes older, after six years.
Long-term medications have their own side effects because it can be
harmful later on in the individual’s life. As febrile convulsions are
self-limiting, ensure that the child is in a safe environment when such
a fit occurs.
Q: In what way can parents or the guardians help the child
when a fit occurs?
A: Unwanted manoeuvres during the time of the fit can endanger
the child’s health and will have dramatic consequences. This can lead to
choking and difficulty in breathing so parents/guardians should be
educated on what to do. The important thing is not to panic and bring
the child to a position lying down (horizontal) in a foetal position.
No external substances should be administered by mouth during the
time of the fit as it can have a dangerous impact. If the fit doesn’t
subside after about five minutes, the child should be taken to the
doctor immediately.
Q: Is there a particular drug which the parents/guardian can
administer at home?
A: Yes, if the fit doesn’t resolve spontaneously within five
minutes, the parent/guardian can administer a medicine called diazepam
which is given through a vial through the rectum.
The child should be kept under observation and consult the doctor on
a frequent basis.
Q: Do febrile convulsions develop into epilepsy later in life?
A: This is very rare but if febrile convulsions prolong for
more than 20 minutes then the chances of developing epilepsy can be
more.
 Even
though febrile seizures are quite benign, every episode should be fully
evaluated by a doctor. A child may have had three febrile seizures from
which they recovered quickly and easily, but the fourth episode of
convulsions and fever may be a serious illness, not febrile seizures. So
it really depends from each child as it can trigger different reactions
in children. Even
though febrile seizures are quite benign, every episode should be fully
evaluated by a doctor. A child may have had three febrile seizures from
which they recovered quickly and easily, but the fourth episode of
convulsions and fever may be a serious illness, not febrile seizures. So
it really depends from each child as it can trigger different reactions
in children.
Q: Do children with febrile convulsions need EEG
(Electroencephalography) and CT (computed axial tomography) scans?
A: Not at all. If the diagnosis of febrile convulsions are
very clear these investigations are not really necessary.
Best is to talk to a doctor first before doing any sort of
investigations.
Q: Do febrile convulsions affect the development of the child?
A: No. A child will develop normally and achieve their full
potential even if they have had febrile convulsions when they were
small.
Breast cancer cells outsmart the immune system and thrive
Scientists have discovered a new way breast cancer cells dodge the
immune system and promote tumor growth, providing a fresh treatment
target in the fight against the disease. While comparable mechanisms to
avoid the immune system have been identified in mice with breast and
other cancers, the study tested human breast tumor cells, putting
researchers closer to understanding how the disease progresses in real
patients.
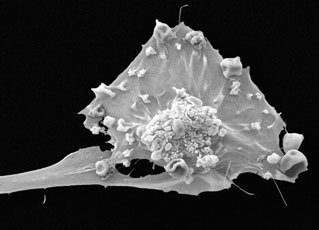 The
study, published in the journal Cancer Research, found high levels of
the protein Hsp27 (heat shock protein 27) are released from human breast
cancer cells and may not only render immune cells unresponsive to the
tumor, but increase blood flow to the tumor as well, both of which fuel
tumor growth. The
study, published in the journal Cancer Research, found high levels of
the protein Hsp27 (heat shock protein 27) are released from human breast
cancer cells and may not only render immune cells unresponsive to the
tumor, but increase blood flow to the tumor as well, both of which fuel
tumor growth.
“Our study is very unique because we used human breast cancer cells,
which are extremely difficult to get,” said Asit De, lead author and
research associate professor in the Department of Surgery at the
University of Rochester Medical Center, who worked closely with
physicians at the Wilmot Cancer Center. “The way tumor cells operate in
mice is not identical to humans, so we need to do more of these types of
human studies to confirm or reject cancer-related discoveries in mice.”
Past research reports Hsp27 is present in high levels inside breast
tumor cells and is associated with resistance to chemo and radiation
therapy. De and his team discovered Hsp27 is also released, or pushed
out of breast tumor cells, into the area surrounding the tumor, known as
the breast tumor microenvironment.
Transform
Once outside the cells, Hsp27 may transform circulating white blood
cells called monocytes that enter the tumor into cells known as
macrophages, which do the opposite of what they are meant to do.
Usually, macrophages work to wipe out tumor cells, but in this case
they help, rather than hurt, tumor cells.
These particular macrophages may make human T cells - the main immune
cells that attack and kill foreign invaders, like tumors - totally
indifferent to the tumor and the body’s call to destroy it.
In addition to suppressing the immune response to the tumor, these
macrophages encourage rapid formation of extra blood vessels that can
help in supplying blood to the tumor - a process known as angiogenesis -
essentially feeding the tumor so it can continue to grow.
Elevated levels of Hsp27 have been found in the blood of cancer
patients with other solid tumors, such as liver and pancreatic cancer
tumors, leading study authors to believe the protein may play a role in
tumor progression beyond breast cancer.
“Our finding that Hsp27 aids tumor progression is just the start - we
know there are several other molecules that help breast tumor cells
suppress the immune system and we hope to identify more of them in
future research,” noted De.
Discovered
A new way to kill cancer - Scientists have discovered a way to kill
cancer cells. Hsp27 is a ubiquitous protein that is important in all the
body’s cells.
When it remains inside cells at normal levels it acts as a chaperone,
protecting cells from stress, such as exposure to high heat or
chemicals.
Only when the protein is let loose outside cells does it appear to
have a detrimental effect on the immune system.
To carry out the study, De worked closely with clinicians in surgical
oncology and plastic surgery at the Medical Center to obtain and analyze
tumor-containing breast tissue samples from breast cancer patients
undergoing surgery and normal breast tissue samples from healthy
volunteers undergoing breast reduction. He also collected and tested
blood samples from untreated breast cancer patients and age-matched
healthy women.
Besides skin cancer, breast cancer is the most commonly diagnosed
cancer among women in the United States.
It is also the second leading cause of cancer-related death in
American women, behind lung cancer.
The development of treatment strategies that stop a tumor’s ability
to silence or circumvent the immune system require a better
understanding of tumors’ various avoidance mechanisms, such as the one
identified by De.
De plans to continue research on Hsp27 in breast cancer, studying
whether blocking Hsp27 slows tumor growth.
Source: Emily Boynton, University of Rochester Medical Center
Parkinson’s disease
Researchers develop new, working mammalian model to combat genetic
causes of Parkinsons:
Evidence is steadily mounting that genetic factors play an important
role in many cases of Parkinson’s Disease (PD). In a study published
February 2, 2011, online in the Journal of Neuroscience, researchers
from the Ecole Polytechnique Federale de Lausanne (EPFL) in Switzerland
report a new mammalian model for studying a specific gene mutation
commonly found in PD sufferers, opening the door to new drugs to fight
the malady.
 “This
is a great step forward toward a more comprehensive understanding of how
the disease works, and how it can be diagnosed and treated,” explains
neuroscientist and EPFL President Patrick Aebischer, lead author of the
study. “This
is a great step forward toward a more comprehensive understanding of how
the disease works, and how it can be diagnosed and treated,” explains
neuroscientist and EPFL President Patrick Aebischer, lead author of the
study.
PD is a common neurodegenerative disease that greatly reduces quality
of life and costs the United States around 23 billion dollars a year.
Until now, researchers have encountered difficulty in reproducing PD
pathology in animals because of an incomplete understanding of the
disease.
Recently, a mutation of the gene coding for LRRK2, a large enzyme in
the brain, has emerged as the most prevalent genetic cause of PD
(genetics are implicated in about 10 percent of all PD cases). When the
enzyme is mutated, it becomes hyperactive, causing the death of
vulnerable neurons and leading to a reduction in levels of the brain
neurotransmistter dopamine. This decrease in dopamine eventually
triggers the symptoms characteristic of Parkinsons, such as tremors,
instability, impaired movement, and later stage dementia.
Now, with funding from the Michael J. Fox Foundation for Parkinson’s
Research, Aebischer and his team in the Neurodegenerative Studies
Laboratory at EPFL, have successfully introduced mutant LRRK2 enzyme
into one hemisphere of a rat brain, resulting in the same PD
manifestations that occur in humans in one side of the rodent’s body.
To do this, the researchers spent two years producing and optimizing
a viral vector to deliver mutated, LRRK2 coding DNA into the rat brain.
LRRK2 is a large and complicated enzyme and designing a vector
capable of transporting its extremely long genetic code was no small
feat.
The new animal model developed by EPFL is sure to benefit future
Parkinson’s research. The fact that LRRK2 is an enzyme - a catalyzing
protein involved in chemical reactions - makes it drug accessible and
therefore of specific interest to researchers looking for
neuroprotective strategies, or pharmaceutical treatments that halt or
slow disease progression by protecting vulnerable neurons. Armed with
the LRRK2 model, new pharmaceuticals that inhibit the hyper-activity of
the enzyme could one day prevent the destructive chain of events that
leads to neurodegeneration and devastation in many with PD.
Source:
Michael Mitchell, Ecole Polytechnique Federale de Lausanne
Arthritis: A degenerative condition
by Dr Jayateerth W Kulkarni
Arthritis is a degenerative condition causing wear of the
articulating surfaces, resulting in pain at rest, pain with movements,
restriction of movements and in severe cases, deformity.
Arthritis and its types
The most common type is osteoarthritis, which is wear and tear
associated with ageing.
It can be accelerated, or aggravated, or even caused by trauma,
excess body weight, obesity, mal-alignment of the joints or congenital
joint deformities (dysplasia).
The other common type of arthritis is called rheumatoid arthritis. In
this disease, the immune system of the body reacts against the joints
and musculoskeletal tissues. This causes inflammation of joints, and
leads to wear and tear.
The other types of inflammatory arthritis are: aukylosing
spondylarthropathy, Lyme disease, gouty arthritis, arthritis associated
with connective tissue disease, psoriasis, inflammatory bowel disease,
etc.
Can arthritis be stopped or reversed?
Once wear and tear has been established, arthritis progresses
relentlessly.
There is no way to stop or reverse arthritis. Certain factors like
weight reduction, activity modification, correcting mal-alignment,
control of inflammation by anti-inflammatory or disease modifying
anti-rheumatic drugs etc. may control wear and tear, but cannot reverse
it.
Certain nutritional supplements like chondroitin sulphate and
glucosamine and other medications like methyl-sulphonyl methane,
esterified fatty acids and diacerin have been shown to have some
beneficial effect on arthritis, but cannot completely cure arthritis, or
reverse the wear and tear process. These are beneficial in early stages
of arthritis, and need to be taken for 3-12 months. They are not
beneficial in advanced arthritis, and neither have they any role in
inflammatory arthritis.
Currently, tissue culture and genetic engineering are being applied
to find a cure for arthritis, but till date, there is no universally
successful technique that has effective clinical applicability. Dr
Jayateerth W Kulkarni is Senior Consultant Orthopedic Surgeon, Apollo
Hospitals, Bangalore.
Courtesy: BPositive
Intermittent drug treatment can curb malaria
WHO estimates that about six billion dollars a year are needed to
wipe out malaria.
The intermittent use of preventive antimalarial drugs can be
beneficial in curbing the spread of the disease in children, according
to the results of a study released Tuesday.
Trials conducted in Mali and Burkina Faso showed that this type of
treatment during the malaria transmission season could reduce infection
rates by between 70 and 85 percent.
The two randomized controlled trials each involved more than 3,000
children who were treated with intermittently with the antimalarial
drugs sulphadoxine pyrimethamine and amodiaquine.
The treatment “provided substantial additional protection against
episodes of clinical malaria, severe malaria, and all-cause hospital
admissions,” said the study reported in the Public Library of Science
journal.
The drug treatment “adds to the benefit of sleeping under bednets”
the report said, adding that “that this public health intervention is
best delivered by community-based, volunteer village health workers.”
The authors of the Burkina Faso study wrote that the results offer
“strong evidence to support the integration of (intermittent preventive
treatment for children) into malaria control strategies in areas of
seasonal malaria transmission.”
The authors of the study in Mali arrived at a similar conclusion,
saying: “These findings indicate that (the drugs) could make a valuable
contribution to malaria control in areas of seasonal malaria
transmission alongside other interventions.”
The research was led by Diadier Diallo from the London School of
Hygiene & Tropical Medicine; Amadou Konate from the Centre National de
Recherche et de Formation sur le Paludisme in Ouagadougou; and Alassane
Dicko from the Malaria Research and Training Centre in Mali.
A third study in Gambia, also noted in the journal, indicated
administering the drugs by community-based, volunteer village health
workers was more effective and less costly than delivery by reproductive
and child health teams run by the Ministry of Health.
The disease killed an estimated 781,000 people in 2009 - including
about 650,000 children aged under five - but that figure has been
reduced from 985,000 in 2000, the World Health Organization said
recently.
International spending in the war on malaria is predicted to peak at
1.8 billion dollars in 2010, but WHO estimates that about six billion
dollars a year is needed to wipe out the disease.
-AFP
|

