|

Body Dysmorphic Disorder and its effect on humans
By Nilma DOLE
Everybody wants to be beautiful and people have long-suffered to make
themselves perfect as society expects. Striving to be beautiful has been
many people's life's goals including young girls who yearn for
model-perfect curves but what happens when it becomes a deadly
obsession? "When I see the many cases of deformities and compare it with
my specialty skin clinic where people want to be fairer or want glossy
hair, I can't believe that people who have everything are not happy,"
said Dr. Jayasiri Jayawardena, one of Sri Lanka's leading Ayurvedha
specialists and consultant at the National Hospital.
 |
|
Low self-esteem
contributes to body dysmorphic disorder |
He said that it becomes difficult to 'cure' these so-called patients
when they are not happy with how they look even after the prescribed
course.
"As a doctor, I generally see three or four cases of deformities a
week but I have at least 10 cases of people who want to look beautiful.
It is difficult that doctors like us have to think of the lucrative
side of making people beautiful but for me, it's talking to patients and
telling them to be happy with what they have," he said.
The condition of not being happy with one's image and the obsession
of being beautiful is known as Body Dysmorphic Disorder (BDD) which is
also called dysmorphophobia.
"A person affected by this condition is extremely worried about
physical appearance and have low self-esteem. They are also very worried
about what others think of their image," he said.
Often in cases where people come to see him for beauty purposes, Dr.
Jayawardena often has a side counselling session where he helps people
talk about their emotions and their perception of their looks.
"Most don't have anything wrong in their body but they want to change
it.
I'm not a plastic surgeon so I feel it's my duty to educate people to
be happy with themselves," he said.
Usually the sufferer complains of many specific features or a single
feature which they are not happy with. This even leads to them not being
happy with their lives, their family and it can even lead to suicidal
behaviour.
"I have noticed depression in certain cases where they have anxiety
and really want to look beautiful or else nothing good will happen.
For example, a rather plump young girl asked me to make her look slim
in a month just because she thought she could have a better suitor for a
marriage proposal," said the doctor.
According to the Psychological Medicine survey, about 1-2% of the
world's population meet all the diagnostic criteria for BDD.
There is no known cause of BDD but it can stem from abuse, neglect or
hidden factors that the sufferer is greatly affected by. Personal
criticism to one's appearance might start as something small or
something someone said but it could cause severe mental strain to the
sufferer.
Common symptoms include loneliness, compulsive behaviour, depression,
anxiety, distance from loved ones, panic attacks, difficult temper,
inability to focus on work or study, comparing with others and low
feelings about themselves.
"We can help patients with BDD by just talking to them and showing
them how beautiful they are. Changes in the environment and how their
loved ones perceive them is important," said the doctor.
In addition to this, psychotherapy, medication, or a combination of
both might help heal the patient. According to research, it has been
proved that Cognitive Behavioural Therapy (CBT) and Selective Serotonin
Reuptake Inhibitors (SSRIs) are effective in treating BDD.
"No matter what we look like, we should be happy with what we have.
Most people don't have arms, legs or even their vital organs intact so
we as healthy individuals should be happy with ourselves," said the
doctor.
Preventing the spread of HIV/AIDS
A new study further validates the use of humanized BLT mice in the
fight to block HIV transmission. The more than 2.7 million new HIV
infections recorded per year leave little doubt that the HIV/AIDS
epidemic continues to spread globally.
That's why there's the need for safe, inexpensive and effective drugs
to successfully block HIV transmission.
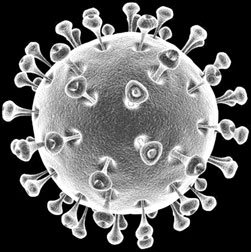 The "BLT" name is derived from the fact that these designer mice are
created one at a time by introducing human bone marrow, liver and thymus
tissues into animals without an immune system of their own. Humanized
BLT mice have a fully functioning human immune system and can be
infected with HIV in the same manner as humans. The "BLT" name is derived from the fact that these designer mice are
created one at a time by introducing human bone marrow, liver and thymus
tissues into animals without an immune system of their own. Humanized
BLT mice have a fully functioning human immune system and can be
infected with HIV in the same manner as humans.
The pioneering developers of the humanized BLT mouse model are Paul
Denton, PhD, instructor of medicine and J. Victor Garcia-Martinez, PhD,
professor of medicine in the UNC Center for Infectious Diseases and the
UNC Center for AIDS Research.
In the study published May 18 in the Journal of Virology, Denton and
colleagues provide data that validates humanized BLT mice as a
preclinical experimental system that potentially can be used to develop
and test the effectiveness of experimental HIV prevention approaches and
topical microbicides.
The animal study reproduced the design and methods of a recent
double-blind clinical study in 889 women of the topical microbicide
tenofovir.
That study, the CAPRISA 004 trial, tested topical pre-exposure
prophylaxis (PrEP) with 1 percent tenofovir which participants were
instructed to apply vaginally twice daily. The 2.5 year trial resulted
in an overall 39 percent reduction in instances of vaginal HIV
transmission. Among women who self-reported as strongly adhered to the
recommended instructions the protection figure climbed to 54 percent.
The new topical PrEP study by Denton and coauthors in humanized BLT
mice reproduced the CAPRISA experimental design with tenofovir. The
researchers say they "observed "88 percent protection of vaginal HIV-1
transmission," which was further confirmed by lack of detectable virus
anywhere in the animals.
The researchers then tested six additional microbicide drug
candidates for their ability to prevent vaginal HIV transmission. These
experimental compounds, not yet tested in people, interfere with the
virus' ability to reproduce. Partial or complete protection was shown by
all but one of these drug candidates. Based on these positive results,
Denton said these inhibitor drugs warrant serious consideration for
future testing in people.
"This animal model has great potential value for testing and
predicting the HIV preventive benefits of the second generation of
microbicide candidates that are aimed at preventing viral replication,"
Garcia said. "The results of these studies will help provide important
information for current and future clinical trials." (Source: Les Lang
University of North Carolina School of Medicine)
New and recurring cancers differ from tumours
When women with a history of breast cancer learn they have breast
cancer again, one of the first questions they and their doctors ask is:
Has my cancer come back, or is this a new case? Now, new data from Fox
Chase Cancer Center suggest that both new and recurring cancers will
differ significantly from the original tumors, regardless of how many
months or years women spent cancer-free, and doctors should tailor
treatment to the specific qualities of the second tumor, regardless of
whether it's old or new.
 Anita Patt, MD, surgical oncology fellow at Fox Chase and lead author
on the study, will be presenting the findings at the 2011 Annual Meeting
of the American Society of Clinical Oncology on Monday, June 6. "There
tends to be a stigma and a lot of anxiety about the word 'recurrence,'"
says Richard J. Bleicher, MD, FACS, attending surgeon at Fox Chase and
senior author on the study. "Sometimes women will worry more if they
believe their original cancer is back, meaning they didn't 'beat it' the
first time around. Anita Patt, MD, surgical oncology fellow at Fox Chase and lead author
on the study, will be presenting the findings at the 2011 Annual Meeting
of the American Society of Clinical Oncology on Monday, June 6. "There
tends to be a stigma and a lot of anxiety about the word 'recurrence,'"
says Richard J. Bleicher, MD, FACS, attending surgeon at Fox Chase and
senior author on the study. "Sometimes women will worry more if they
believe their original cancer is back, meaning they didn't 'beat it' the
first time around.
These findings suggest they should not get hung up on that idea,
because any subsequent diagnosis - whether it's a recurrence or a new
tumor - will look significantly different from their first cancer."
In women with a history of breast cancer, doctors often approach new
tumors differently depending on whether they believe it's a recurrence
of the first tumor, or a totally new one, Bleicher explains. But there
are no official ways to distinguish between the two types, so doctors
typically rely on a few criteria, then form their own opinion based on
an "overall gestalt," he says.
One of the criteria doctors have used to distinguish between new and
recurring cancers is the amount of time women spent cancer-free,
reasoning that the longer the time between the two tumors, the more
likely the second one is to be an entirely new case. To investigate if
this and other criteria indeed distinguish new and recurring tumors,
Bleicher, Patt, and their colleagues looked at data collected from 4,420
women with a history of breast cancer.
Two-hundred and thirty five women were eventually diagnosed with
another tumor in the same breast, suggesting it could be a recurrence.
However, when the researchers compared the first and second tumors,
they saw that 89% differed in at least one key characteristic that could
potentially affect treatment or prognosis, regardless of whether the
second tumors were new cases or a recurrence of the original cancer.
Sixty percent of the second tumors differed from the first by at least 2
or more criteria, including whether or not it would respond to hormones,
how it was diagnosed, and whether at least 25 percent of the tumor was
confined to the ducts, and therefore less able to spread throughout the
body.
Half of the women experienced a second tumor within 60.5 months of
their first. And, importantly, the amount of time they spent cancer-free
appeared to have no bearing on whether the two tumors differed in any
key characteristics.
The findings suggest that patients and doctors shouldn't spend much
time determining if the second tumor is a recurrence of the first, or a
totally new entity, says Bleicher, and should instead tailor treatment
to the specific qualities of the second tumor, regardless of whether
it's old or new.
"When a patient comes back with a relapse, whether it's a new tumor
or a recurrence, it really doesn't make a difference," he says. "We
treat them both as potentially curable."
(Source: Diana Quattrone Fox Chase Cancer Centre)
Simple fitness test could predict long-term risk for heart attack
How fast can you run a mile?
If you're middle-aged, the answer could provide a strong predictor of
your risk of heart attack or stroke over the next decade or more.
In two separate studies, UT Southwestern Medical Centre researchers
have found that how fast a middle-age person can run a mile can help
predict the risk of dying of heart attack or stroke decades later for
men and could be an early indicator of cardiovascular disease for women.
In one recent study in the Journal of the American College of
Cardiology, researchers analyzed the heart disease risk of 45-, 55- and
65-year-old men based on their fitness level and traditional risk
factors, such as age, systolic blood pressure, diabetes, total
cholesterol and smoking habits. The scientists found that low levels of
midlife fitness are associated with marked differences in the lifetime
risk for cardiovascular disease.
For example, a 55-year-old man who needs 15 minutes to run a mile has
a 30 percent lifetime risk of developing heart disease. In contrast, a
55-year-old who can run a mile in eight minutes has a lifetime risk of
less than 10 percent.
"Heart disease tends to cluster at older ages, but if you want to
prevent it, our research suggests that the prescription for prevention
needs to occur earlier - when a person is in his 40s and 50s," said Dr.
Jarett Berry, assistant professor of internal medicine and a
corresponding author on both studies.
Researchers in this study found that a higher fitness level lowered
the lifetime risk of heart disease even in people with other risk
factors.
In a separate study in Circulation, UT Southwestern researchers found
that the same treadmill test predicts how likely a person is to die of
heart disease or stroke more accurately than assessing the risk using
only typical prediction tools such as blood pressure and cholesterol
levels.
Heart disease is a leading killer in industrialized nations and the
No. 1 killer of women in the U.S. Women younger than 50 are particularly
difficult to assess for long-term cardiovascular risk.
"Nearly all women under 50 years of age are at low risk for heart
disease," Dr. Berry said. "However, as women get older, their risk
increases dramatically. In our study, we found that low levels of
fitness were particularly helpful in identifying women at risk for heart
disease over the long term."
For decades, scientists have tried to improve their ability to
determine which patients are at highest cardiovascular disease risk.
Blood-based and imaging techniques have been used to try to improve
risk prediction, but fitness has not been examined until now, Dr. Berry said.
For both studies, researchers collected information from thousands of
participants who underwent a comprehensive clinical exam and a treadmill
exercise test at the Cooper Clinic in Dallas between 1970 and 2006.
In the JACC study, researchers evaluated more than 11,000 men tested
before 1990 - women were excluded because of the low number of
participants and cardiovascular death rates - and found 1,106 who died
of heart attack or stroke during the study period. They measured
participant fitness levels and traditional risk factors for heart
disease. Within each age group, higher levels of fitness were associated
with lower levels of traditional risk factors.
For the Circulation study, researchers examined more than 66,000
participants without cardiovascular disease, ages 20 to 90. They were
then followed until death or the end of the study period; follow-up
lasted up to 36 years. There were 1,621 cardiovascular deaths during the
study. The researchers found that by adding fitness to the traditional
risk factors, they significantly improved their ability to classify
participants' short-term (10 years) and long-term (25 years) risk. |

