
Immunisation, the key to measles prevention
By Carol Aloysius
Currently a targeted number of 200,000 infants between six months to
one year are being immunised throughout the island with all MOH clinics
opened to cope with the demand.
|
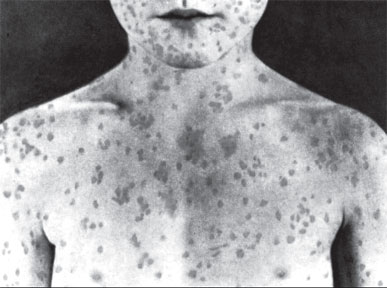
Measles spots on a child's body |
Measles remains one of the leading causes of death among young
children globally, despite the availability of a safe and effective
vaccine. Approximately 158,000 people died from measles in 2011
worldwide - mostly children under the age of five, according to recent
World Health Organisation (WHO) estimates. The disease, which is widely
rampant in most third world countries with transmission favourable
environments and overcrowding, has achieved a significant reduction of
cases and deaths in Sri Lanka.
Due to the successful immunisation program, the nation experienced
very low measles transmission for the past 14 years.
However, recently, an increasing number of measles cases has been
observed throughout the country, the highest numbers reported from the
Western Province.
Consultant Epidemiologist of the Epidemiology Unit, Ministry of
Health, Dr Deepa Gamage, explains in an interview with the Sunday
Observer, the cause of this recent outbreak, how it can be controlled,
and most importantly, how the disease can be prevented using available
local resources.
Excerpts of the interview ….
Question: The Epidemiology Unit last week initiated a
countrywide national immunisation program against measles, targeting
200,000 infants between six months to one year. We are told that this is
because several cases of measles have been reported to the Unit from
many are in the country, especially in the Western Province. What is the
cause for this sudden increase in the number of cases of measles?
Answer: Highly contagious diseases such as measles are likely
to get outbreaks from time to time. This is a usual experience in any
country.
Accumulation of possible susceptible people from time to time leads
to outbreaks cyclically.
Q. There was a fear among mothers sometime ago when there were
reported cases of severe allergies to the rubella vaccine. Many even
stopped taking their children for their normal immunisation against
mumps, measles and whooping cough. Is this one of the reasons for the
sudden surge in measles, after 14 years of keeping the figures at a new
low in Sri Lanka?
A. This is not identified as a reason for the vaccine
withdrawals of that incident. It is true that we have faced some
temporary threat to National Immunisation Program due to that incident.
But with collaborative effort of all, corrective measures were taken to
maintain high Immunisation coverage for Measles and Rubella throughout
the country.
By analysing age groups it is obvious that most affected are from one
year and above 30 years during this current experience of increased
measles transmission situation.
Q. What causes measles? Is it a virus or bacteria?
A. Measles is caused by a virus (Paramyxovirus in genus
Mobillivirus)
Q. Who are most at risk? Infants? toddlers? Adolescents?
Youth? Elderly? Why?
A. Any age group is at risk of getting measles infection if
they do not have immunity for protection. But young age categories
(infants and toddlers) are prone to get complications if they get
measles infection due to their low immune systems.
Q. What are the symptoms? Is high fever the first symptom?
A. Fever may or may not be the first symptom. Initial
prodromal period with malaise, respiratory symptoms (cough and runny
nose), fever, conjunctivitis (red eyes) will follow the skin rash
(maculo popular).
Q. Since rashes on the skin are a symptom how are these rashes
different from other rashes that babies develop like allergy rashes or
chicken pox?
A. Chicken pox rash is different. It is a vesicular rash.
Allergic rash is usually itchy but sometimes, some allergies might mimic
this. There may be some other infections also present with fever and
similar rashes. But in a clinically suspected case of measles,
considering clinical signs and symptoms, laboratory confirmation
facilities are available (Virology Laboratory, Medical Research
Institute) for the final diagnosis for measles, and should be done at
this elimination stage.
Q. How does it spread?
A. It spreads by air from one person to the other (aerosol),
and enters through the respiratory tract and oropharynx to a susceptible
person
Q. Can it be prevented? If so how?
A. Vaccination against measles to increase immunity against
measles infection and prevention of contact with an infected person are
the best methods for preventing measles. With regard to the second
method of prevention of contact by isolation i.e. keeping the infected
person separate from others, this can be adopted only after knowing the
person is infected.
However, one must remember that an infected person can transmit the
infection even during incubation period (time period from the time the
virus enters into the body to the onset of the first symptom).
The period of communicability (time period in which the infection can
spread to others) is four days before the onset of the measles rash to
four days after onset of rash.
Vaccination for measles is thus the most recommended method in
prevention of measles.
Q. The measles vaccine is often incorporated with rubella and
mumps vaccines in countries where these illnesses are problems. Is this
being done in Sri Lanka as well? Since when, and why?
A. The measles component is incorporated with Mumps and
Rubella in the vaccine of MMR. Sri Lanka has been using MMR vaccine
since October 2011. Due to low transmission of measles disease and
considering additional protection for mumps, Sri Lanka is currently
using MMR in our National Schedule. MMR is given at the age of one year
and three years as two doses per child in our National Schedule.
Q. When should one seek professional medical advice?
A. If any patient becomes more unwell and prone to
complications, he/she needs to seek medical advice. Parents of all
infants are advised to seek medical advice as infants are more prone to
get complications. Others with risk factors like Immunodeficiency
status, malnutrition, especially Vitamin A deficiency, and during
pregnancy, are also advised to seek medical advice without delay.
Q. Are there varying degrees of measles from mild, to moderate
to severe?
A. This will depend on the individual and the risk factor
status. The severe or mild form will depend on the immunity development
ability of the individual and underlying risk factor status of the
individual.
Q. What are the complications when it reaches the severe
stage?
A. Ear problems (Otitis media)
• Respiratory tract complications such as Pneumonia, and bronchitis
• Diarrhoea
• Eye problems: Blindness due to Vitamin A deficiency and Keratitis
• Nervous system complications : Encephalitis, and a condition called
Sub Sclerosing Pan Encephalitis (SSPE)
Q. How do you treat this disease? Is there a specific
treatment?
A. There is no specific treatment for measles. Mainly
symptomatic supportive treatment is given.
Most patients with uncomplicated measles will recover with rest and
supportive treatment. If complications occur they need to be treated
accordingly.
Q. Can a mother treat her child at home? If so, what are the
home remedies?
A. For children with measles, usually home remedies are not
recommended and we strongly recommend getting medical advice.
However, until the visit to the doctor, control of fever, maintenance
of hydration and maintenance of nutrition is advisable.
Q. When is hospitalisation required?
A. If the patient’s general health is deteriorating even after
medical advice and with supportive treatment, hospitalisation is
required.
Q. Where is it most likely for measles to break out in
epidemic form? Are poor communities living in unsafe unhygienic
environments more at risk than others?
A. Measles transmission is more in highly populated areas.
Since this is respiratory spread, crowding is the major factor but poor
hygienic environments facilitate transmission.
Q. What role does nutrition, healthy diets and vitamins play
in (a) preventing the disease (b) minimising the effects in children
with compromised immune systems?
A. Nutrition, a healthy diet and Vitamin A, may prevent
development of complications and manifestation of severe complications.
(Eg: if child with vitamin A deficiency, contacted measles he/she may
end up with blindness).
Q. Whereas previously only one dose of measles vaccine was
given to children by their first birthday, I understand the WHO has now
recommended two doses of the vaccine to ensure immunity and prevent
further outbreaks.
Your comments with reference to Sri Lanka?
A. Yes, that is true. In our National schedule in Sri Lanka
also we are giving two doses of measles, at the completion of one year
and at the completion of three years since 2011(October) Before that
Measles was given at nine months of age and MR(Measles-Rubella vaccine)
was given at three years of the age [still two doses of measles
containing vaccines since 2001]. Before 2001, Measles 1 dose was given
at the age of nine months since 1984.
Q. The Fourth Millennium Development Goal (MDG 4) aims to
reduce the under five mortality rate by two thirds between 1990 and
2015. Is measles eradication included in this program? Since only one
year is left to reach this target, will Sri Lanka be able to eradicate
or reduce the measles burden in time?
A. MDG 4 aims at reducing under-five childhood mortality. This
is by reducing deaths caused by six diseases, of which one is Measles.
We have achieved that target already.
For Measles, the current global and regional strategy is Measles
Elimination.
We have still not moved on to Eradication stage as in Poliomyelitis.
The Measles Elimination is planned in Sri Lanka by 2018 on par with the
Regional Elimination strategies.
Our elimination target is to reduce measles cases for five per
million population and zero mortality by 2018.
Q. Your message to the public especially to parents on 1)
Prevention – via immunisation etc 2) Precautions and treatment?
A. We have identified increased measles transmission during
this year with high proportion among six to 12 months age group.
Supplementary immunisation activity or additional vaccination dose of
measles has been planned and given to all children of 6-12 months (born
between July 6 2012 to January 5 2013) through Maternal and child health
clinic centres of all Medical Officer of Health (MOH) areas as a measles
disease control activity.
If any child has not been given this Measles vaccination, parents are
requested to get their children vaccinated if they belong to this age
category. The Central clinic of the MOH office on July 13, 20 and 27
(Saturdays) is open to vaccinate these children.
All the children who have received measles vaccinations through this
special campaign are advised to continue with routine MMR vaccination.
This special measles vaccination is given as an additional
vaccination irrespective of the age appropriate routine vaccination.
****************
Key facts on Measles from WHO
• Measles is one of the leading causes of death among young children
even though a safe and cost-effective vaccine is available.
• In 2011, there were 158 000 measles deaths globally - about 430
deaths every day or 18 deaths every hour - mostly children under five
years.
• More than 95 percent of measles deaths occur in low-income
countries with weak health infrastructures.
• Measles vaccination resulted in a 71 percent drop in measles deaths
between 2000 and 2011 worldwide.
Measles is a highly contagious, serious disease caused by a virus. In
1980, before widespread vaccination, measles caused an estimated 2.6
million deaths each year.
****************
What the Centre for Control of Diseases says…
Measles is a serious respiratory disease caused by a virus. It
spreads easily through coughing and sneezing. In rare cases, it can be
deadly.
The measles, mumps, rubella (MMR) vaccine protects against measles.
Symptoms
•Measles starts with a fever, which can get very high.
•Soon after, it causes a cough, runny nose, and red eyes.
•Then a rash of tiny, red spots breaks out. It starts at the head and
spreads to the rest of the body.
•The rash can last for a week, and coughing can last for 10 days.
****************
War against mosquito-borne diseases continues
In the global war against disease-carrying mosquitoes, scientists
have long believed that a single molecular door was the key target for
insecticide.
This door, however, is closing, giving mosquitoes the upper hand. In
Proceedings of the National Academy of Sciences, a team of researchers
has discovered a second gateway that could turn the tide against the
mosquitoes’ growing advantage.
For many years, pyrethroid insecticides have been deployed in
developing countries to fend off diseases such as malaria, dengue fever
and more. They're so effective that they are the only insecticides the
World Health Organization uses with their mosquito nets they distribute
around the globe.
 “Pyrethroids are effective because they eliminate mosquitoes while
having few if any side effects on humans,” said Yuzhe Du, MSU
electrophysiologist and one of the lead authors. “Pyrethroids are effective because they eliminate mosquitoes while
having few if any side effects on humans,” said Yuzhe Du, MSU
electrophysiologist and one of the lead authors.
“Our discovery of a second receptor in the mosquitoes’ sodium channel
gives us a better understanding of how the insecticide works at a
molecular level as well as could lead to ways to stem mosquitoes’
resistance to pyrethroids.”
Receptors on sodium channels act as doorways. Pyrethroids work by
propping open the sodium channel. Mosquitoes don't die from the toxin,
per se. They die from sodium overdose. With the door jammed wide open,
their cells gulp down sodium, which overexcites their nervous system and
eventually leads to paralysis and death.
In the past decade, growing resistance in mosquitoes has been
detected in many countries. At the molecular level, resistance appears
as mutations in the primary receptor in the sodium channel that allow
mosquitoes to survive exposure to the insecticide. The discovery of the
second receptor in the sodium channel, however, opens up more avenues to
increase pyrethroids’ effectiveness.
“One of the keys to the success of this research was our cloning of a
mosquito sodium channel for the first time,” said Ke Dong, MSU insect
toxicologist and neurobiologist and the paper's senior author.
“Another lead author of this study, Yoshiko Nomura, dedicated nearly
one year to make this happen, which allowed Dr. Du to perform
electrophysiological experiments with the clone.”
The team then spent nearly two years to discover the new
pyrethroid-binding site, she said.
The revelation not only explains much of pyrethroid resistance found
in mosquitoes worldwide, but also helps answer why they affect insects
but not humans and other mammals. Since this is a growing issue with
cockroaches, bedbugs, fleas, potato beetles and other crop pests, the
discovery could lead to benefits for the pest-control industry and
farming.
MNT
Baby born after revolutionary IVF technique
A baby boy has been born following a revolutionary IVF technique that
allowed doctors to screen large tracts of his DNA for chromosome defects
that would have prevented the embryo from implanting successfully into
his mother’s womb.
It is the first time that scientists have used whole genome
sequencing to test for defects in IVF embryos that are not apparent from
visual inspections. The technique could help to improve the success rate
of IVF cycles, making it easier for some couples to have children.
 The boy, is healthy and normal. Another American woman who underwent
the same procedure is also pregnant and about to give birth, said Dagan
Wells of the Biomedical Research Centre at Oxford University, who helped
to develop the technique. The boy, is healthy and normal. Another American woman who underwent
the same procedure is also pregnant and about to give birth, said Dagan
Wells of the Biomedical Research Centre at Oxford University, who helped
to develop the technique.
Abnormal chromosomes are one of the single biggest problems that
prevent IVF embryos from successfully implanting - and probably the main
reason why about 80 percent of IVF embryos fail to develop into
full-term, healthy pregnancies.
“Chromosome abnormalities are about tenfold greater in number in
humans than in any other species we know of. As chromosome abnormalities
go up, implantation rates go down in almost a mirror image of one
another,” Dr Dagan said.
Previous research suggests that testing IVF embryos for chromosomal
abnormalities before implantation can improve success rates by a third
and reduce miscarriages by a half, Dr Dagan will tell the European
Society of Human Reproduction and Embryology, meeting in London.
The technique, called “next generation sequencing”, uses DNA machines
to decipher the genetic code of millions of strands of DNA taken from a
single cell of the embryo extracted when it is about five days old.
This reveals whether there are abnormal numbers of chromosomes, or
cases where parts of a chromosome are deleted, Dr Dagan said. Doctors
used the technique to screen the DNA of seven embryos from the couples
undergoing IVF. The women were aged 35 and 39 and one couple had a
history of miscarriage.“Many of the embryos produced during infertility
treatments have no chance of becoming a baby because they carry lethal
genetic abnormalities. Next generation sequencing improves our ability
to detect these abnormalities and help us to identify the embryos with
the best chances of producing a viable pregnancy,” Dr Dagan said.
“In the past few years, results from randomised control trials have
suggested that most IVF patients would benefit from embryo chromosome
screening, with some studies reporting a 50 percent boost in pregnancy
rates.
- The Independent
|


