|

The secret of longevity:
A heart healthy lifestyle
By Carol Aloysius
Heart diseases have soared in recent years claiming the lives of
younger and younger patients in the prime of their lives. Once
considered a disease of the elderly, heart disease, like every other non
communicable disease in this country, has overtaken the number of
communicable diseases, with victims as young as in their forties,
thirties and even late twenties.
|

Coronary angiogram in progress at the Sri Jayewardenepura
General Hospital Cardiac catheterisation laboratory |
The rat race for survival, stresses and strains of modern lifestyles,
unhealthy eat-on-the-run lunches and dinners dripping with saturated
fats, high in cholesterol and salt, lack of exercise and tendency to put
off visiting a physician till the last moment even when there are
warning signs: All these are contributory causes for what is today, Sri
Lanka's number 1 killer disease. Health officials however have
repeatedly emphasised that heart disease is preventable, by following a
few simple rules.
Consultant Cardiologist, Sri Jayewardenepura General Hospital, Dr.
NAOMALI AMARASENA explains what these rules are, and tells us how to
detect and prevent heart disease in this interview with the Sunday
Observer.
Excerpts...
Q. Coronary heart disease (CHD) is currently listed as one of
the leading non communicable diseases in Sri Lanka. Is this a recent
phenomenon? If so why?
A. Cardiovascular disease makes up over 25 percent of all
deaths for the South Asian region to which Sri Lanka belongs. This is
not a recent phenomenon. However with better control of infectious
diseases including the virtual eradication of diseases such as malaria
and filaria, non communicable diseases such as coronary disease, stroke
and cancers have come to the forefront as the leading cause of mortality
and morbidity in the past two decades.
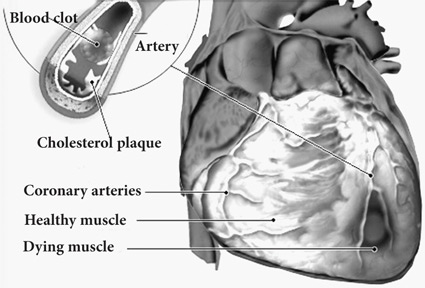
Q. How is it caused?
A. Coronary artery disease is caused by hardening of the
arteries or atherosclerosis. This means that fatty deposits called
plaque build up inside the arteries. Atherosclerosis can affect any
arteries in the body.
When it occurs in the arteries that supply blood to the heart it is
called coronary artery disease. When plaque builds up in the coronary
arteries, the heart doesn't get the blood it needs to work well. This is
called Ischaemia. Ischaemia can cause symptoms such as chest pain on
exertion known as angina. If a plaque tears, the body tries to fix the
tear by forming a blood clot around it. The clot can block blood flow to
the heart and cause a heart attack.
Q. Are there different forms of CHD? If so what are they?
A. I would rephrase it as different forms of heart disease.
These are Coronary Artery Disease, Valvular Heart disease as a
consequence of rheumatic fever, and Congenital Heart Disease.
 Q. Who is most at risk? Is old age a bigger risk factor than
having an NCD such as hypertension or diabetes? Q. Who is most at risk? Is old age a bigger risk factor than
having an NCD such as hypertension or diabetes?
A. Both hypertension, hiperlipidaemia and diabetes are major
risk factors for coronary artery disease. Diabetes particularly is known
as a coronary artery disease equivalent. Although increasing age is a
risk factor by itself, coronary artery risk is multifactorial with both
modifiable risk factors (i.e. smoking, lifestyle and obesity) and non
modifiable risk factors (i.e. gender, age and family history). Your
chance of getting coronary artery disease rises with the number of risk
factors you have.
Q. I read that in recent years our hospitals are seeing more
and more younger patients admitted with symptoms of heart disease. The
majority are also males. Your comments?
A. Coronary artery disease is very rare in males too young to
drive, but begins to creep up after men are old enough to vote! As many
as 10 percent of all heart attacks occur before the age of 45 and most
of these strike men.
After puberty insulin resistance and triglycerides rise in males and
HDL (known as the good cholesterol) levels fall, while girls enjoy
opposite and protective changes. Hormones account for some of this, but
so do health habits.
Teenage boys and young adult males are known to smoke more and eat
more fast foods than girls although I am not too sure that the latter is
now true in Sri Lanka! Also after leaving school the amount of exercise
they get starts to decrease.
Q. What is the outlook for these young heart attack patients?
A. The short term outlook for heart attack victims younger
than 45 is actually better than for older patients, perhaps because they
often have single vessel disease and well preserved heart muscle.
But a heart attack is just the tip of the atherosclerosis iceberg,
and without dramatic interventions, the disease is likely to progress.
In one study of men and women who were stricken before age 40, only one
percent died within a year, but 25 percent died in less than 15 years.
Q. What are the symptoms? How can they be identified early?
A. The most common symptoms of CAD are angina and shortness of
breath when exercising or doing other vigorous activity. Women are
somewhat more likely than men to have other symptoms such as nausea,
back or jaw pain. Angina symptoms include chest discomfort (pressure or
a strange feeling in the chest). This feeling can be in other areas such
as the arms, neck, jaw or back. Angina can be stable or unstable. Stable
angina has a typical pattern. You can likely predict when it will
happen. It usually occurs when your heart is working harder and needs
more oxygen such as during exercise.
Q. Do the symptoms pass?
A. Symptoms go away when you rest or take glyceryl trinitrate
(tablets or spray.) Unstable angina is a change in your usual pattern of
stable angina. It is a warning sign that a heart attack may soon occur.
It is an emergency. Some people don't have any symptoms. This is called
Silent Ischaemia. In some cases particularly in diabetics you can even
have a silent heart attack i.e. a heart attack without symptoms.
Q. What is the treatment?
A. There are many medications that your physician can
prescribe to lower blood pressure, cholesterol, optimise diabetes
management and control symptoms of angina. Lifestyle modification i.e.
eating a heart healthy diet, weight reduction and regular exercise is an
important part of the treatment'.
If medication, diet and exercise alone, are not effective in treating
the disease. If arteries become blocked, coronary angioplasty with
stenting or open heart surgery may be performed.
Q. How successful are these treatments?
A. Both coronary angioplasty and coronary artery bypass
surgery work by improving the blood supply to the heart. One by clearing
a blocked artery with a metal tube. The other by bypassing the block by
using conduits (veins and arteries) from the patients own body.
 Both these treatment modalities are very successful in relieving the
symptoms. But unless the risk factors which led to the problem are
successfully addressed there will be disease progression with further
blocks occurring. Both these treatment modalities are very successful in relieving the
symptoms. But unless the risk factors which led to the problem are
successfully addressed there will be disease progression with further
blocks occurring.
Q. Is this procedure used for all blocked and narrowed
arteries?
A. Not all the blocked or narrowed arteries can be stented or
grafted (if they are too small in calibre). Thus a few patients may
experience anginal chest discomfort after the angioplasty or bypass
surgery which may be disheartening.
Usually these arteries are not significant in terms of the patients
prognosis and adequate reassuarance as well as optimising anginal drug
therapy will be required.
A graded exercise program will lead to development of collaterals
(growth of new arteries bypassing the block) which will lead to relief
of symptoms.
Q. Any new breakthrough in treating heart patients?
A. All modalities of treating coronary artery disease are
aimed at relieving symptoms and slowing the progression of the disease.
There is no complete cure for CAD. That would be the ultimate
breakthrough in treating CAD patients.
However all other modalities i.e. medication, stenting and coronary
artery bypass surgery (CABG) are constantly being improved upon with
more effective drugs with fewer side effects, stents which are easier to
implant and which last longer and improvement in CABG techniques.
The facilities available for investigating this disease has also
improved considerably over the past decade.
Q. How can heart disease be prevented?
A. Let me give you some easy to follow rules:
* Lower your blood pressure
* Eat a heart healthy diet
* Regular physical exercise and medication
*Quit smoking and avoid exposure to second hand smoke
* Control diabetes
* Improve your cholesterol - high levels of LDL and total cholesterol
increase your risk of heart disease and high levels of HDL protect
against heart disease - exercise and a healthy diet low in unhealthy
fats are also important ways of lowering the cholesterol.
* Maintain a healthy weight - exercise and a weight reducing healthy
diet may help. May need to obtain the assistance of a dietitian.
*Eat right - low fat high fibre diet including fresh fruit and
vegetables and whole grains.
*Reduce stress - take time out every day for a few quiet minutes to
unwind and appreciate life.
*Manage anger - seek ways to control feelings of anger and hostility.
Q. Once patients are discharged from hospitals after surgery,
can they lead a normal life? Can they go back to their former jobs or
has there to be a change in occupations if they are employed in jobs
that require a lot of hard manual labour?
A. Immediately after a bypass operation the patient should
participate in a cardiac rehabilitation program. In most cases the
patient can get back to his/her former job after around six weeks or
even sooner if they have had an uncomplicated post operative course. It
takes six to eight weeks after surgery for complete healing of the
breast bone. If they are employed in jobs requiring hard manual labour
they may have to consider a change in occupation.
Q. Can they climb stairs, sweep the house, do gardening, drive
their car?
A. Yes. In fact they climb stairs before discharge from
hospital!
Q. What about their sexual functions? Can they resume normal
sexual relationships?
A. Yes, after recovering after the effects of surgery - wound
healing etc. However, sexual problems shortly after a bypass surgery are
common. Both men and women may have less sex or feel less satisfied with
sexual activity. A variety of factors may contribute including side
effects of drugs (such as beta blockers), depression and fears about
triggering a new heart attack or dying. In such a situation exercise
testing can be used to determine if a person is at any risk of heart
problems related to sex.
Q. Apart from adults children also have various congenital
heart diseases such as hole in the heart etc. How do these defects occur
and when? While still in the mother's womb or after birth?
A. Congenital heart defects are problems with the hearts
structure that are present at birth. Common examples include holes in
the inside walls of the heart and narrowed or leaky valves. In more
severe forms, blood vessels or heart chambers may be missing, poorly
formed or in the wrong place.
Q. Can these defects be corrected while still in the womb
using new techniques like keyhole surgery etc?
A. Most defects can be corrected after the child is born.
Foetal cardiac intervention has only a few indications i.e certain
defects such as a critically narrowed valve which will lead to the death
of the foetus and is also amenable to interventional techniques.
Appropriate patient selection involves the evaluation of not only the
foetal cardiac defect but also the maternofoetal aspect and the
pregnancy as a whole.
Q. What are the symptoms of congenital heart disease?
A. Many defects such as a small atrial septal defect (a common
type of hole in the heart) have no symptoms at all. However the general
signs include: excessive sweating, extreme tiredness and fatigue, poor
feeding, rapid heart beat, rapid breathing, shortness of breath, chest
pain and a blue tinge to the skin (cyanosis.)
Q. How are they managed? Can they be looked after at home?
A. Only the infants who need immediate surgery are kept in
hospitals. These are the infants with complex congenital heart disease
incompatible with an independent life without surgical or catheter based
intervention. All others can be discharged home and brought back for
either corrective or palliative surgery as the case may be at the
appropriate time.
Q. Some parents tend to over-protect children who are detected
with murmurs. Your comments?
A. Most murmurs (abnormal heart sounds) in infants and
children are innocent. However they should be subjected to an
echocardiogram to exclude any congenital heart disease. Parents with
children with congenital heart disease should be counselled. They should
also be strongly advised not to neglect the other healthy children in
the family.
Q. Is Rhuematic fever also a heart disease?
A. Rheumatic fever is an inflammatory disease that can develop
as a complication of inadequately treated sore throat caused by a
particular strain of Streptococcus bacteria. The patient has fever and
painful, red, hot and swollen joints. It is a disease that 'licks the
joints and bites the heart'. Not all patients with rheumatic fever
develop Rheumatic heart disease which is its most dangerous
complication. Once rheumatic heart disease develops the patient will
need long term treatment and follow up as well as life long prophylaxis
from further attacks of rheumatic fever.
Q. Finally, describe what you would call a healthy balanced
diet 1) for patients 2) to avoid heart disease using locally available
vegetables, fruits etc. Is a vegetarian diet preferable or one with fish
and lean meat?
A. Cut out saturated and trans fats - reduce solid fats like
butter or hard margarine. Trim fat off any meats. Change your lifestyle
by snacking on fruits and vegetables instead of chips! Unsaturated fats
are essential for good health. Fatty fish eg. salmon. Canola oil,
vegetable oils, peanuts, cashew and avocados are good sources of these
fats (use in moderation.) Focus on high-fibre foods - brown rice, whole
wheat pasta. Eat a variety of fruits and vegetables (diabetics though
should seek advice on which fruits to eat as well as the quantities).
Don't leave out the legumes - add peas or lentils to soups. Reduce salt
in your food - ideally one teaspoon a day. Steer clear of processed
foods (they all have added salt).
Q. Any suggestions for substitutes?
A. If you switch to substitutes, opt for healthy substitutions
e.g. semi-skimmed milk for full cream milk, soft margarine for butter,
lean meats like chicken and fish for red meats.
Q. Any heart-healthy cooking methods?
A. For heart healthy cooking methods: bake, broil, lightly
stir fry and saute using small amounts of vegetable or olive oil.
Positive messages better at persuading smokers to quit
Which is more likely to convince a smoker to quit? The words,
"Warning: cigarettes cause cancer beneath the image of an open mouth
with a cancerous lesion and rotten teeth, or the same image with the
words, "Warning: Quitting smoking reduces the risk of cancer"?
The answer depends on how confident you are in your ability to quit,
according to a study led by researchers at Georgetown Lombardi
Comprehensive Cancer Center. The research, which involved 740
participants and three D.C. Area institutions, suggests that a mix of
messages might work best to help convince some of the 45 million smokers
in the U.S. to give up the habit, says the study's lead investigator,
Darren Mays, a Georgetown Lombardi population scientist who specialises
in behavioural cancer prevention.
The study found that "gain-framed" messages - those that stressed the
benefits in quitting, such as "quitting smoking reduces the risk of
death due to tobacco" - were more effective for smokers who believed
quitting would be hard.
On the other hand "loss-framed" messages - the ones that emphasised
the negative outcomes from smoking, such as "smoking can kill you- were
more effective for smokers who thought they could quit when they wanted.
Most of the warnings used now on tobacco packages in the U.S., and
worldwide, are loss-framed messages, which may not be sufficiently
convincing to many smokers, says Mays. "This study shows us that
leveraging both gain - and loss-framed messaging may prompt more smokers
to quit," he says. Mays and his colleagues undertook the study to build
the evidence base for the new graphic warnings proposed for U.S.
cigarette packages.
The 2009 Family Smoking Prevention and Tobacco Control Act authorised
the U.S. Food and Drug Administration (FDA) to regulate tobacco
products, and required new pictorial labels for cigarette packs.
Tobacco industry lawsuits, however, have delayed implementing the new
pictorial warning labels, and in 2012, the U.S. Court of Appeals struck
down the nine pictorial warnings proposed by the agency.
The FDA is currently pursuing additional research to support
implementation of the warning label requirements. Mays and colleagues
chose to study the impact of four pictorial pictures - a man using a
breathing apparatus; two sets of lungs, one healthy and one diseased; a
prone man with stitches on his chest lying on a white sheet; and the
cancerous mouth - with loss-frame or gain-framed messages. Each was
effective. "Leveraging policies such as graphic warnings for cigarette
packs to help smokers quit is critical to improve public health
outcomes. Our study shows that that framing messages to address smokers'
pre-existing attitudes and beliefs may help achieve this goal," says
Mays.
- MNT
|

