|
Health wise
Enlarged prostate gland:
No need to fear
by S. Anandakumar
Prostate although a commonly used medical term, was rarely discussed
in public, in the good old days. However, nowadays, no eyebrows are
raised, when you hear someone say, “I have an enlarged prostate”!
 Now, the term “Prostatitis” (inflammation or enlargement) rings a
bell alright among the men folk, but is rarely understood. Perhaps, due
to misconceptions surrounding this medical disorder, one tends to rush
to conclusions with his own diagnosis and some with grand motherly
treatment. Now, the term “Prostatitis” (inflammation or enlargement) rings a
bell alright among the men folk, but is rarely understood. Perhaps, due
to misconceptions surrounding this medical disorder, one tends to rush
to conclusions with his own diagnosis and some with grand motherly
treatment.
To put things in its proper perspective, the Sunday Observer “health
wise” presented the case to two eminent genito-urinary tract specialists
in the country, Dr. Srinath Chandrasekera, Consultant Urological Surgeon
and Senior Lecturer in Surgery of the Sri Jayawardenapura University and
Dr. Suren de Zylva, Consultant Urological Surgeon, Colombo North Medical
College Hospital, Ragama.
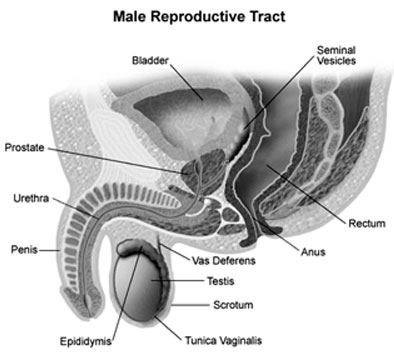
The walnut-sized prostate gland found in the genito-urinary tracts of
males, surrounds the urethra just below the urinary bladder. The gland
produces semen, the milky white fluid that nourishes and transports the
sperms, through the prostatic urethral, during sexual excitement
(orgasm).
Both specialists, while discussing the prostate and its maladies,
allayed fears of men with this common and highly prevalent. disorder
that could be treated with least inconvenience.
The male hormone, testosterone is very essential for a male to lead a
normal, and healthy life. But, at the same time, the very same healthy
testosterone which, from mid 30’s to 50’s is in ample production, tends
to be an attributing factor in the enlargement of the prostate. This
swelling compresses the urethra and partially blocks the urine flow.
Symptoms of enlargement of the prostate can be easily detected, when
a person:-
(i) Finds it difficult to pass urine.
(ii) Hesitancy in the onset; initiation; slowness in dribbles; longer
periods to empty the bladder; process completed with a strain; and at
the end, the feeling of incompleteness.
(iii) Sudden urgency to pass urine.
(iv) Frequent increase at nights.
(v) Incontinence (No muscle control)
Due to one or more of these conditions, complications will set in due
to retention of urine, which may necessitate the patient to be
hospitalised, to facilitate the free flow of urine with the help of a
catheter. Recurrence of this condition may lead to infection, which may
result in bleeding.
The pressure developed in the urinary system, may lead to kidney
ailments, which could be best avoided, if the symptoms are taken
seriously.
The specialists were emphatic that sexual abstinence has no direct
association with prostate related complaints.
While highlighting the minor consequences due to negligence to
observe and take treatment the doctors also caution that ABSENCE of
these symptoms does not mean that one does not have prostatic problems.
The message that urologists want to convey is that any normal healthy
looking male who has the symptoms, to consult his physician who may
refer the case to a specialist to be medically evaluated. After
recording the history the patient will be subjected to a simple,
painless procedure known as Digital Rectal Examination (DRE). And the
cancer detection test-the Prostate Specified Antigens (PSA) will confirm
whether the inflammation (Swelling) is benign (non-carcinogenic) or
malignant (carcinogenic).
The initial treatment, barring major complications, in the opinion of
the two urologists, is to opt for:
(i) Relax the prostate with alpha blockers which gives relief for 24
to 48 hours.
(ii) Shrink the prostate (in the case of larger ones) - relief for
six-12 weeks.
If neither of the two procedures is not successful it will be decided
to go for the common methods, through the natural orifice using the
latest technique, the TURP. The Trans Urethral Resection of Prostate (TURP)
is a time-tested, cost effective, and easily available surgery in all
major hospitals (including State-run institutions).
This surgery rarely leads to any complications.
Due to gross negligence on the part of the patient, if the prostate
is allowed to grow slightly larger than usual, the specialists advocate
the latest in medical technology - the laser method, which in their
parlance is known as “Bloodless” procedure.
The most wonderful aspect is when the patient with a complaint of
enlarged prostate gets rid of the prostrate is discharged on the same
day and reports for duty at his workplace, the very next day!
It is that simple!
Sri Lanka’s Bypass heart surgery:
A paper to be presented at Taipei Medical Congress
by Edward Arambewala
A paper on a recent study done in Sri Lanka on the baseline
characteristic differences in Coronary Artery Bypass Grafting (CABG)
surgery between the State and private sector hospitals is to be
presented at the 17th annual sessions of the Asian Society for
Cardiovascular and Thoracic Surgery (ASCVTS) to be held in Taipei Taiwan
next month, March 5-8.
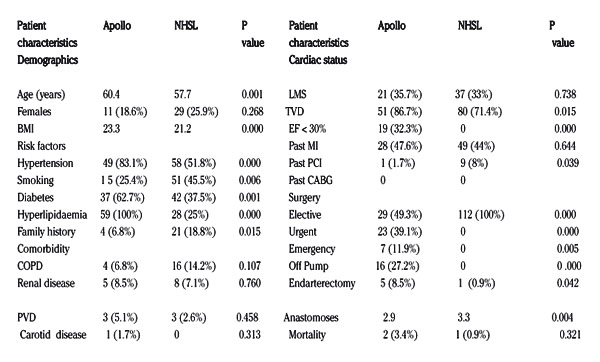
According to this study, it has been found that the patients
undergoing CABG in the private sector are older and have a significantly
higher BMI and poorer myocardial function, needing for more emergency
operations and off pump CABG when needed.
The combined medical team to present the paper at the conference,
which has also been responsible for this study is being led by Colombo
Apollo’s Cardiothoracic Surgeon Dr. Sujeeth Suvarna and the others
comprise Drs. Tolusha Harischandra, Thilan Walgamage and Saman Basnayake.
Dr. Suvarna in an interview with the Sunday Observer said: “In this
study we retrospectively reviewed the case records of all consecutive
patients who underwent isolated CABG in a single centre at Apollo
Hospital, Sri Lanka from June to October, 2008 and we compared this data
with the data published in 2008 of the clinical profile of CABG patients
at the Colombo National Hospital Sri Lanka (NHSL) and we compared the
data of 59 patients who underwent CABG at Apollo with 112 patients who
underwent surgery at the NHSL.
A brief outline of the paper :
Background: A recent study of CABG in the Government sector of Sri
Lanka established its baseline characteristics as being different from
that of the current trend in developed countries. However, whether this
is true in the private sector, which handles half the CABG work load of
the country, is unknown. Therefore the objective of this study was to
establish the present status of CABG in the private sector of Sri Lanka
in comparison to that of the Government sector.
Methods: We retrospectively reviewed the case records of all
consecutive patients who underwent isolated CABG in a single centre at
Apollo Hospital, Sri Lanka from June to October, 2008. We compared this
data with data published in 2008 of the clinical profile of CABG
patients at the National Hospital of Sri Lanka (NHSL).
Results: The 59 patients who underwent CABG at Apollo were compared
with the 112 patients at the NHSL.
Conclusion: Patients undergoing CABG in the private sector are older
and have significantly higher BMI, hypertension, diabetes and
hyperlipidaemia, smoking is significantly less. They have poorer
myocardial function and undergo more emergency/urgent operations and off
pump CABG when needed. These findings have implications for risk
reduction strategies and training requirements.
|
Results: The 59 patients who underwent CABG at Apollo were compared with the 112 patients at the NHSL.
 |
|
BMI (Body Mass Index), COPD (Chronic Obstructive Pulmonary Disease),
PVD (Peripheral Vascular Disease), LMS (Left Main Stem), TVD (Triple
Vessel Disease), EF (Ejection Fraction), PCI (Percutaneous Coronary
Intervention) |
Cardio - Pulmonary resuscitation (CPR)
By Dr. D. P. Atukorale Cardiac arrest
Sudden cardiac arrest (SCA) is a leading cause of death in all the
countries and is due to ventricular fibrillation (VF) ventricular
tachycardia (VT) or due to cardiac asystole (CA). Results of
resuscitation are very much better in patients with VF or VT as compared
to patients with cardiac asystole.
 The common causes of cardiac arrest are heart attacks, trauma, drug
overdosage, electric shock and drowning and asphyxia in case of
children. The common causes of cardiac arrest are heart attacks, trauma, drug
overdosage, electric shock and drowning and asphyxia in case of
children.
Cardio -Pulmonary Resuscitation (CPR)
Three to five minutes of collapse can produce survival rate as high
as 49% to 75%. As soon as you come across a collapsed person (with
cardiac arrest) you must call for help and start immediate CPR.
Look for regular chest movement and if the collapsed person is
breathing there is no immediate necessity to start mouth to mouth (or
mouth to nose) respiration. If the victim is not breathing and if the
pulse is not palpable start cardiac massage with rescue breathing
without delay. The procedure of C. P. R. is given below;
(a) Open the airway
Lift the chin with one hand, push down on the forehead with the other
hand to lift the head back. Remove any foreign bodies in the mouth such
as dentures and pull the tongue out if the tongue is interfering with
respiration.
(b) Breathing
If the patient is not breathing, give the victim mouth-to-mouth (or
mouth-to-nose respiration). Place your mouth over the patient’s mouth
(or nose) so that no air can escape. Give two or three breaths into the
mouth or nose. Majority of people who give C P R prefer mouth to nose
respiration as far as I am aware.
(c) Check the Carotid pulse
Place your hand on the patient’s carotid artery (next to the Adam’s
apple in the neck) and check for the carotid pulse. If there is no pulse
begin cardiac massage immediately.
Cardiac Massage
Kneel beside the patients chest. Find the sternum, the breast - tone
where both sides of the rib-cage meet and place your hands on the
sternum. Bring your shoulders over the victim’s chest, keeping your arms
straight. Press down on the sternum about one to two inches. Then relax
the sternum and let the sternum rise back to the normal position. But do
not remove your hands from the chest.
Give 15 - 20 such compressions for every two breaths you give. You
must give about 100 compressions per minute.
In case of cardiac arrest (when the heart has stopped pumping blood)
hypoxia (lack of oxygen) to brain begins to occur in about four to five
minutes after the cardiac arrest. Brain death usually occurs after eight
to ten minutes and CPR should be ideally started in the first five
minutes of arrest as permanent brain cell damage or death of brain cells
would have occurred in about ten minutes after arrest.
When you start CPR you must always call for help and arrange for an
ambulance. After giving CPR for about 20 minutes most people get
exhausted and you must get the help of another person, until the
ambulance arrives.
With effective CPR the chest expands and the pulse can be felt.
Continue with chest compression and rescue breathing in the rates of 30:
2 continue resuscitation (CPR) until qualified help arrives and takes
over and until the victim breaths normally. If normal respiration does
not start, get the help of another person if you are exhausted.
Risk to the rescuer
In Sri Lanka where pulmonary tuberculosis is still common there is
the risk of the rescuer getting TB, HIV infection is a problem but it is
very rare.
So it is advisable for the rescuer to use his or her handkerchief
during mouth-to-mouth or mouth-to-nose respiration so that victims mouth
or nose does not come into direct contact with the rescuer. In Sri
Lanka, as far as I am aware many children do not receive CPR because of
rescurer’s fear of causing harm to the victim. This fear is unfounded
and CPR should always be done in case of children. Readers will agree
with me that it is better to have a live child with a few rib fractures
than to have a dead body without fractures. For lack of space. I am not
discussing CPR in case of children in this article.
Immediate CPR and defibrillation (electric shock to the heart) within
three to five minutes of collapse can produce survival rates as high as
78%.
As soon as you come across a person with cardiac arrest you must call
for help and start immediate C P R until an ambulance arrives. Look for
regular chest movements and if the collapsed person is breathing, there
is no immediate indication for starting mouth-to-mouth or mouth-to-nose
respiration.
As mentioned earlier if the victim is not breathing and if carotid
pulse is not palpable, cardiac massage with rescue breathing should be
started immediately.
With effective ventilation, chest will expand. Blow into the victim’s
mouth or nose twice and then give about 20 chest compression. Continue
with chest compression and rescue breathing in a ratio of 30:2. If the
victim starts normal breathing continue with the chest compression.
Continue C P R until qualified help arrives and takes over. If you are
exhausted give over C P K to another person.
Common mistakes
I have come across hundreds of patients brought with history of
cardiac arrest during the 23 years I served the Institute of Cardiology.
National Hospital and majority of the victims were dead on admission as
in almost all these unfortunate cases they had not been given
mouth-to-mouth (or mouth-to-nose) respiration during the transport of
the victim to Coronary Care Unit.
Only cardiac massage had been given. Some of the readers of the
article may have observed in the TV that in case of almost all the
victims brought by ambulances for admission to National Hospital,
Colombo, during the period the victim is transferred from the ambulance
to the I.C.U., the nursing staff who takes over the victim give cardiac
massage but the staff rarely give mouth-to-mouth respiration.
As I mentioned earlier mouth-to-mouth (or mouth-to-nose) respiration
is a must if the patient is not breathing.
Results of C P R
Results of resuscitation in case of patients warded in C C U are
excellent especially, in case of primary ventricular fibrillation,
thanks to the efficient nursing staff and doctors in the C C U, who work
as a team.
I can remember 62 years old female patient who had been resuscitated
successfully for cardiac arrest in 1974.
This fortunate lady who was a famous maths teacher, lived upto the
ripe old age of 95 years after discharge from hospital and passed away
two years ago. The above patient was brought to C C U in a collapsed
state by a family physicians who had given both cardiac massage and
mouth-to-mouth respiration; during transport of the patient in an
ambulance. |


