|
Health Wise
March 13 is World Kidney Day:
Kidney transplant offers longer life to CKD patients
Transplant success rate over 90 percent in Sri Lanka:
By Carol Aloysius
With kidney disease now rampant in the island, the surge in the
number of patients who have reached stage 5 level of the disease has
raised serious concerns among kidney specialists.
 For these patients dialysis treatment is the main option. Chronic
kidney disease (CKD) patients on dialysis requires a minimum of twice a
week treatment to survive. The treatment is not only costly and a hassle
to patients making that bi-weekly trek to the hospital, it prevents them
from leading a quality life. For these patients dialysis treatment is the main option. Chronic
kidney disease (CKD) patients on dialysis requires a minimum of twice a
week treatment to survive. The treatment is not only costly and a hassle
to patients making that bi-weekly trek to the hospital, it prevents them
from leading a quality life.
So what is the other option they have?
Kidney transplants will definitely give them a longer quality life
says an expert in the field, who cites global studies on the subject to
prove his argument. He says that unlike dialysis treatment which is
hampered by the limited facilities in our hospitals, there are plenty of
kidneys to go around, if the kidneys from brain dead patients admitted
to hospitals could be donated to these critically ill dying patients. A
kidney transplant will give them a new lease of life and save lives. The
need of the hour is more donors of live kidneys”, says Sri
Jayawardenepura hospital Consultant Nephrologist Dr Chinthana
Galahitiyawa who explains why kidney transplants are a better option for
chronic kidney patients in this interview with the Sunday Observer.
Excerpts...
Q. As kidney disease is widely prevalent, what are the most
common kidney diseases one finds in our country?
A. Diabetic kidney disease, Hypertensive kidney disease,
Chronic kidney disease of Unknown aetiology, Glomerulonephritis, and
Polycystic kidney disease.
Q. What are the most severe health risks they carry?
A. Kidneys are the main controller of body water content,
electrolyte concentration (ex Potassium, Sodium, chloride) Acid
Base\balance. Kidneys are responsible for clearing up nitrogenous waste
products from the body. Kidneys also mediate blood pressure control, and
secrete a hormone called Erythropoetin to stimulate bone marrow to
produce red blood cells. Additionally, they contribute in vitamin D
production.
Q. What happens when there is kidney failure?
A. Complete or partial malfunction of the kidney functions is
called kidney failure.
In kidney failure all above mentioned functions will get disturbed.
This results in failure to control the water content and patients
developing swelling (Oedema) of the body.
Wet lungs might lead to shortness of breath. Electrolyte imbalance is
a major issue and it can be lethal. Specially high potassium levels can
cause cardiac arrest in a short time period. Rising body acidity is
detrimental to all cellular functions.
Q. What are the main symptoms? How are they caused?
A. Accumulation of waste products such as ammonia, urea and
creatinine in the body is the main reason for the so called “uraemic”
symptoms in kidney patients. These include loss of appetite, nausea,
hiccups, vomiting, lack of sleep, itching of the body, lack of energy,
change in skin colour and drowsiness. Blood pressure rises and becomes
uncontrollable. Red blood cell production reduces and patient might
develop anaemia. Kidney disease population in general is calcium and
vitamin D deficient.
When all these problems derange the body composition it becomes life
threatening. Apart from these direct problems in kidney failure, it puts
the patient at a higher risk for ischemic heart disease (coronary artery
disease).
The majority of the chronic kidney disease patients will die of heart
attacks than from the end stage kidney failure.
Q. Is it irreversible?
A. Yes, it's irreversible. Chronic kidney disease is a slow
progressive loss of kidney functions over the months to years.
Q. How does treatment help?
A. It will help to slow down the progression of the disease
and to minimize the metabolic derangements. Treatments are helpful to
alleviate the symptoms and improve the quality of life.
Q. How do you treat it?
A. Control the underlying disease ex-Diabetes, Blood Pressure.
Avoid further damages ex- avoiding kidney damaging medicines such as
strong pain killers in the class of NSAID, certain antibiotics and radio
contrast dies used in angiography and CT scans.
Proper measured fluid intake to avoid dehydration and regular medical
follow ups and good quality water consumption are also important here.
Q. What is end-stage renal disease? How do you treat patients
who have reached this stage?
A. Kidney functions are classified according to Estimated
Glomerular Filtration rate (EGFR). This is calculated using patients
creatinine level, age, gender and body weight.
Normal EGFR is 90 to 110. CKD is classified in to 5 stages according
to the EGFR value. End stage is EGFR is less than 15 and the patient has
symptoms and signs of “uraemia”, where he needs renal replacement
therapy for the survival.
This includes blood or peritoneal dialysis or kidney transplant.The
usual pattern is to educate the patient and the family well before they
reach the end stage. There the patient is prepared for a renal
replacement therapy (RRT) or continued with conservative care.
Those who wish to have haemodialysis needs a arteriole-venous fistula
(AVF) created to get the needle access for dialysis. For patients
planning to have peritoneal dialysis can get a peritoneal dialysis
catheter inserted to their abdomen.
Once these measures are done the patient can wait till they actually
need RRT and have the treatment when it is needed. Patients need
replacement of calcium and stimulation for red cell production by
erythropoietin injections regularly. Further they need regular diabetic
and blood pressure control medications.
Q. You mentioned that patients with stage 5 kidney disease had
two options: dialysis or kidney transplant. Which is the better option
and why?
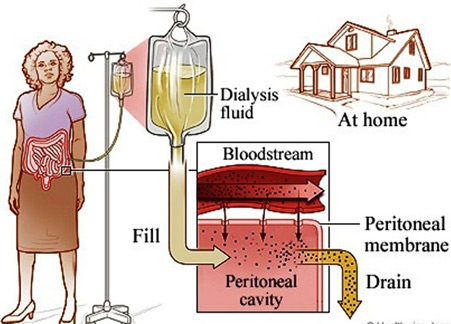
A. Dialysis is the process where another mechanism purifies
patient's blood in place of his/her own kidneys.
This is mainly of two types. Haemodiadialysis where actually the
blood is sent in to a machine for cleaning and send back to the patient.
In peritoneal dialysis a special fluid is instilled in to the peritoneal
cavity and that removes the toxins and extra water from the body.
Once these dialysis processes purify the patients uraemic toxins and
controls the water content regularly, patients can live a reasonably
good quality life. But they will require dialysis for the rest of their
lives.
They will need to have regular well organized and monitored dialysis
program. The only option to stop this is by having a transplanted
kidney.
Q. Compared to dialysis, are kidney transplants better for the
patients?
A. World wide data confirms that the patients live longer with
kidney transplants than with dialysis. Their quality of life and
fertility is much better with transplants. Further, patients have much
more freedom with transplants as they are less restricted in diet and
also they don't spend time bound to dialysis machines. Cost-wise too it
is advantageous.
Q. Drugs after a transplant-are they also given free to
patients in state hospitals?
A. In Sri Lanka all transplant medicines are given freely from
the government hospitals.
 They need to continue these immune suppressants indefinitely. But
with time this may be cut down to a minimum. They need to continue these immune suppressants indefinitely. But
with time this may be cut down to a minimum.
Regular maintenance haemodialysis however is not freely available to
all the patients due to the heavy demand at the public sector hospitals.
Therefore many patients have to bear the cost of dialysis at private
sector.
Q. Once a person gets a new kidney, how long will it remain in
his body if it doesn't reject it?
A. It will remain for longer periods and the usual Sri Lankan
life span or a renal allograft is more than ten years.
Q. Does the age of the patient or the donor have any
significance in the success of a transplant?
A. Yes, we usually take kidneys from age compatible donors.
Young kidneys work better!
Q. Are there side-effects after a transplant? What are they?
A. Many patients gain weight and some can develop diabetes.
They are more prone to catch infections than the general population.
They should be on a normal calorie diet with less salt.
The best option is to meet a qualified dietitian to get a suitable
individualized diet devised. Regular exercises are advisable for all the
patients to keep their sugar, blood pressure and weight at optimum
levels.
Q. Since kidney transplants are a better option, do we have
enough spare kidneys to round?
A. Unfortunately no. Most of the patient's family members are
also suffering from similar diseases such as diabetes, high blood
pressure and polycystic kidney disease.
Further their blood groups are not always compatible. Because of
these reasons we have a huge deficit of live donor kidneys.
At Sri Jayawardenepura Hospital alone, we have more than twenty
patients who are in need of a kidney transplant but without suitable
donors at the moment.
We also have roughly 3,000 kidney patients visiting our OPDs, many of
them might need a kidney transplants in the future.
Q. What is the success rate of these transplants?
A. Sri Lankan transplant rates are compatible with those of
the western countries. It is about 90 percent successful in the first
year.
Q. Will kidney transplants be the future approach to treating
end stage chronic kidney failure patients?
A. It has already established its place as the preferred
modality in end stage kidney disease.
In Sri Lanka we have the skills and equipment to do these transplants
successfully, but we need more donor kidneys, which is our main
obstacle. We also need to develop more transplant centres to cater to
the rising numbers of patients.
Q. Any message to the public regarding this issue?
A. We have planned to establish a national cadaveric kidney
donation program to fill the deficit in the future.
We hope to conduct island wide awareness programs to motivate people
sign up necessary documents to donate their organs in case of sudden
deaths to be utilised for the benefit of these long suffering patients.
A special program to raise awareness on this subject will be held at
Maligawatte Nephrology Dialysis Centre On March 13 from 8 a.m. to 12
noon.
Protect your kidneys
by Dr. Nadeeka K. Rathnamalala
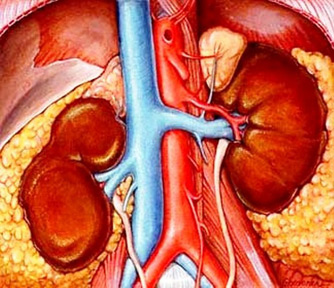
The kidneys are amazing organs that do many essential tasks to keep
us healthy. Each kidney is roughly the size of your fist and is situated
deep in the abdomen. The kidney consists of about a million tiny
functional units called the nephrons. The main job of the kidneys is to
remove toxins and excess water from blood. Kidneys also help control
your blood pressure, to produce red blood cells and to keep bones
healthy.
 Kidneys control the level of minerals in the blood such as sodium and
potassium and also help maintain the acidity in the blood. Although only
about 1.5 litres of urine is produced a day, the kidneys filter nearly
180 litres of blood daily. Kidneys control the level of minerals in the blood such as sodium and
potassium and also help maintain the acidity in the blood. Although only
about 1.5 litres of urine is produced a day, the kidneys filter nearly
180 litres of blood daily.
Chronic Kidney Disease (CKD)
When there is progressive loss of function of kidney over months to
years it is known as Chronic Kidney Disease.
Many of the tests that are available detect this at a fairly advanced
stage as some of these tests may still be in the normal range until 50 %
of the combined function of the kidneys is lost. When the tiny filters
or the nephrons are damaged they shut down.
Initially when it is only a few nephrons, the others are able to take
on a greater work load and compensate for it. It is when this
compensation can no longer take place that the effects are seen.
Serum creatinine is the most widely used test that uses blood to
estimate the kidney function.
As this marker starts to go above the normal range only after 50
percent of kidney function is lost we now combine it with a calculation
known as the estimated glomerular filtration rate (eGFR). Testing your
urine for the presence of abnormal amounts of proteins is another way of
detecting kidney problems.
This is especially useful if you are diabetic in which the presence
of albumin (a protein component in blood) in urine is the earliest sign
of kidney damage.
Stages of CKD
As kidney disease progresses slowly, it has been categorised in to
five stages with stage five named End Stage Renal Failure (ESRF).Not
everyone progresses from stage 1 to 5 as in some the progression will be
very slow and they may never reach ESRF.
Burden of CKD
About 1 in 10 people have some degree of CKD. It can develop at any
age and various conditions can lead to CKD. Kidney disease can affect
people of all ages and races. African Americans, Hispanics, American
Indians and people of South Asian origin (those from India, Bangladesh,
Sri Lanka or Pakistan) have a higher risk of CKD. This risk is due in
part to high rates of diabetes and high blood pressure in our part of
the world.
CKD can occur at any age, but it becomes more common with increasing
age and is more common in women. Although about half of people aged 75
or more have some degree of CKD, many of these people do not actually
have diseases of their kidneys; they have normal ageing of their
kidneys. Simple blood and urine tests can detect CKD and simple, low
cost treatments can slow the progression of the disease, reduce the risk
of associated heart attacks and strokes and improve quality of life.
According to the Global Burden of Disease study, in 1992, CKD ranked
27thin the list of causes for deaths in the world while in 2010 it
ranked 18th. This degree of movement was second only to that of HIV and
AIDS. As the prevalence of this disease is increasing dramatically, it
poses an enormous financial burden on health systems worldwide.
According to recent reports the National Health Service in United
Kingdom spends more on kidney disease than breast, lung, colon and skin
cancer combined. In Australia, the cost of treating all current and new
cases of End Stage Renal Failure (ESRF) is estimated at $12 billion. In
China, the economy will lose US$558 billion over the next decade due to
effects on death and disability attributable to chronic cardiovascular
and renal disease.
High blood pressure and diabetes are the leading causes of CKD. High
blood pressure causes over a quarter of all cases of kidney failure.
Diabetes has been established as the cause of around one-third of all
cases.
Other less common conditions include inflammation (glomerulonephritis)
or infections (pyelonephritis). Sometimes CKD is inherited (such as
polycystic disease) or the result of long-standing blockage to the
urinary system (such as enlarged prostate or kidney stones).
Some drugs can cause CKD, especially some pain-killing drugs
(analgesics) if taken over a long time. There are situations where the
cause for the CKD cannot be determined like in the case of the kidney
disease in the North central Province in Sri Lanka.
Treating CKD
There is no cure for CKD however, treatment can slow the progression
and prevent certain complications.
The main treatments are modification of diet and medications in early
stages which would help maintain the balance normally maintained by the
kidneys. When one reaches ESRF the options available are dialysis and
transplantation.
Dialysis is an artificial method of achieving the balance maintained
by the kidneys by excreting unwanted products and excess water. However
this lacks some of the other functions maintained by the kidney such as
the role in production of red blood cells, maintenance of mineral
balance in bones and blood pressure regulation. There are two main forms
of dialysis.
Hemodialysis is widely used in Sri Lanka where the patient is
connected through bloodlines to a machine through which the blood is
cleaned and put back in to the body. To maintain a balance to have an
acceptable quality of life at least 12 hours on the machine is needed
distributed through the week. As the patient needs to come in to a
dialysis centre to receive this form of dialysis and each session
usually spans over four hours, the patient comes in three times a week.
The other form of dialysis which is still not widely available in Sri
Lanka is known as Continuous Ambulatory Peritoneal Dialysis (CAPD). In
this method the lining of the abdominal cavity which is called the
peritoneum acts as a sieve that gets the waste products out of the body.
The patient fills the abdomen with a fluid through a tube that is placed
in the abdominal cavity, after which an exchange takes place between the
blood vessels supplying the wall and the fluid. The fluid is removed
once it is saturated with the waste products from the blood. This is a
home based therapy and the patient can even walk around and carry out
his day to day activities while having fluid in the abdomen. Both these
forms of dialysis do not cure kidney disease, instead they help maintain
an acceptable quality of life.
Kidney transplantation
Kidney transplantation is considered the best treatment option for
most people with kidney disease as the quality of life and survival is
better than those on dialysis. It is an operation where a healthy kidney
is placed in a person with poorly functioning kidneys. A kidney can come
from a living relative, a living unrelated person, or from a person who
has died (deceased or cadaver donor); only one kidney is required to
survive. In general, organs from living donors function better and for
longer periods of time than those from donors who are deceased.
Overall, transplant success rates are very good. Transplants from
deceased donors have an 85 to 90 percent success rate for the first
year.
Preventing CKD
Early diagnosis of CKD enables certain preventive measures to be
taken which have been proven successful through substantive research.
Testing for kidney disease if you have high blood pressure, diabetes, a
family history of kidney disease or overweight can help prevent or delay
kidney disease. Key preventive measures that have been defined are
· Controlling blood pressure - tighter the control within the normal
range lesser the decline in kidney function
· Specific medications - e.g. ACE inhibitors
· Reducing salt intake
to lower blood pressure
·Control of sugar
and lipids
·Cessation of smoking
·Control of weight
·Increasing physical
activity
The writer is Senior Registrar in Nephrology, National Hospital of
Sri Lanka
|

