|

Panacea for all 'devils'
National Poisons Information Centre:
by Shanika Sriyananda
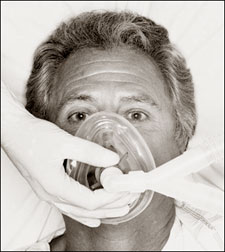 The National Poisons Information Centre (NPIC) of the National
Hospital, which was established with the aim of reducing untimely tragic
but preventable deaths among young men and women in Sri Lanka, is 20
years old now. The National Poisons Information Centre (NPIC) of the National
Hospital, which was established with the aim of reducing untimely tragic
but preventable deaths among young men and women in Sri Lanka, is 20
years old now.
Prof. Ravindra Fernando who was the brainchild of this Centre in an
interview said that one major step that could be taken to prevent
morbidity and mortality from poisoning was to improve the treatment
facilities in State hospitals.
Following are the excepts of the interview:
Q: Why did you establish the National Poisons Information
Centre?
A: During my internship at the General Hospital, Colombo, I
observed tragic, untimely suicidal deaths of young men and women by
ingesting poisons, for most trivial reasons.
I was very disturbed and concerned. Sometimes, I helplessly watched
them dying as we did not have antidotes, drugs, relevant knowledge or
back up services to help them. These events led me to develop an
interest in the field of poisoning or what is termed as 'Clinical
toxicology'.
When I was doing my post graduate studies in the Dept. of Forensic
Medicine at the Guy's Hospital Medical School of the University of
London, I had an opportunity to associate closely with the National
Poisons Unit the first such unit established outside the United States
of America.
When I returned to Sri Lanka after my postgraduate training, I was
determined to start a poisons information centre here, which was not an
easy task.
Q: You mentioned the word 'toxicology'. What is toxicology?
A: Toxicology is the science of toxins or poisons. Toxicology
can also be defined as the discipline that integrates all scientific
information to help preserve and protect health and the environment from
the hazards presented by chemical and physical agents.
 Toxicology is certainly not a new science. Toxicology is certainly not a new science.
Early humans learned about the harmful properties of plants, insects,
venomous snakes and chemicals through experience. Men utilised some of
the toxic plants to incapacitate or kill animals (Arrow poisons).
The Sanskrit documents Rig Veda , written between 1500 and 1200 BC
and Ayurveda, written about 700 BC which also mentions poisons and
antidotes.
Q: How can one get training in toxicology?
A: In 1980s toxicology was not a speciality subject for which
training or postgraduate degrees were available in Sri Lanka. A couple
of years ago, I started a multi-disciplinary post-graduate diploma in
toxicology in the University of Colombo for medical officers and
scientists.
This year, we will commence an 'internet-based' Master of Science
degree in clinical toxicology in the Post Graduate Institute of
Medicine, (PGIM) for doctors.
Q: Is poisoning a major problem in Sri Lanka?
A: Yes, certainly. The table below shows the number of
poisoning cases admitted to the hospitals in Sri Lanka and the number of
deaths. Poisoning is the sixth leading cause of death in our State
hospitals.
In this Table, 'other poisons' include plants and chemicals in
industrial and household products.
According to Police statistics, about 3000 die from suicidal
poisoning every year. Therefore, poisoning is a grave health problem.
Also a grave socio-economic problem only a few people have realised.
What was the commonest age group of patients who take poisons?
Analysis of the enquiries to the Centre showed that about 50% of the
patients belonged to 15 to 30-year group.
This is the commonest age group who consumes poisons to commit
suicide in this country. They are the youth of very productive age
group.
Q: Why does a country need a Poisons Information Centre?
A: Even in developed countries like the United States of
America and the United Kingdom, healthcare professionals usually do not
have a thorough knowledge of toxic ingredients contained in various
pesticides, natural toxins and household and other chemicals.
Although medical professionals are aware of toxic effects and adverse
effects of drugs, their knowledge is limited regarding management when
patients present with ingestion of chemicals and envenomations with
poisonous snakes and plants.
This is why poison information centres were established in developed
countries - to provide quick, accurate and tailor-made information on
toxic ingredients of poisons, their chemical effects and complications,
and management of patients presenting with poisoning.
After our Centre was established, other countries in the region such
as India, Nepal and Pakistan have also established Poisons Information
Centres.
Q: What is the role played by the Poisons Centre in the last
two decades?
A: The Centre has answered nearly 10,000 queries from doctors,
paramedical personnel and the general public during this period. Over
94% enquiries were on management of poisoned patients.
Over 90% of the callers were doctors in State hospitals. Over one
third of the enquiries were on pesticide poisoning while nearly one
fourth were for drug overdoses.
Q: Apart from answering queries from doctors what else does
the Centre do?
A: The Centre has published several books, brochures, leaflets
and posters to educate doctors and the general public.
Seminars, conferences and workshops have been held for different
groups of health care professionals and non-medical personnel who can in
turn disseminate knowledge on first aid and prevention of poisoning. In
July 1997, the Centre was able to host the first SAARC meeting on
poisoning in Colombo.
For the first time in the history of this country the Centre
organized a "National Poisons Prevention Week" in May last year with the
full cooperation of the Minister of Health. The Centre plans to have a
similar week in May this year.
Q: What can be done to reduce morbidity and mortality from
poisoning in this country?
A: One specific action that can be taken to reduce morbidity
and mortality from poisoning is to improve the treatment facilities in
State hospitals. The mortality from pesticide poisoning is still
unacceptably high, varying from 8% to 11%. Non-availability of intensive
care facilities, essential drugs, and other equipment seems to be a
problem in some hospitals.
The Presidential Task Force on 'Formulation of a National Health
Policy' suggested certain measures to reduce morbidity and mortality
from pesticide poisoning in 1993.
One was to strengthen the National Poisons Information Centre.If this
recommendation is implemented, an efficient high quality 24-hour
information service for healthcare professionals can be provided with
laboratory back up service to analyse blood, urine and stomach contents
of poisoned patients to assist doctors in the management.
The Centre can also have facilities to supply antidotes to hospitals.
These activities alone can help to reduce the rising incidence of
morbidity and mortality from poisoning.
[email protected]
Hospital Admissions and Deaths from Poisoning - 2005
Total Hospital Admissions Hospital Deaths
Organophosphates and Carbamate insecticides 12 587 892
Other Pesticides 4 323 378
Therapeutic drugs 18 174 152
Snake bites 36 727 134
Other poisons 17 456 230
Total 89 267 1 786
Alcohol without harming yourselves
by Dr. R. A. R. Perera, Consultant Psychologist.
People of many cultures learn to enjoy the taste of alcoholic drinks,
and the rituals and social situations that are built around their
consumption. Alcohol is substance that is drunk because it induces
feelings of increased confidence and relaxation.
 A significant proportion of the population of most countries is
employed in manufacture, retailing or other enterprises linked to
alcohol, and many national exchequers rely heavily on alcohol taxation.
These are the difficulties, which must be remembered when producing
public health advice on drinking. A significant proportion of the population of most countries is
employed in manufacture, retailing or other enterprises linked to
alcohol, and many national exchequers rely heavily on alcohol taxation.
These are the difficulties, which must be remembered when producing
public health advice on drinking.
Recently, attention has focused on the effects of alcohol on physical
health and here, too, there are some benefits. A 12-year study
(1978-1990) done in United States of America on 276,802 men aged 40, 59
it was found that, men who drink little alcohol had a much better chance
of avoiding death from certain diseases like heart disease and stroke.
People who drink lot of alcohol and those drink none had high rate of
death from heart disease and stroke. The people who drank more had a
higher death rate from diseases like liver diseases, accidents and some
cancers.
Much attention has focused on how alcohol consumption affects the
risk of heart disease which accounts for a large fraction of deaths
among males between 40-60 years of age.
It is difficult to escape the conclusion that alcohol confers some
protection against heart disease. The suggestion that alcohol has a
heart protective action is also plausible.
Alcohol increases; high-density (good cholesterol) cholesterol levels
and reduces fibrinogen levels and platelets, (which causes stickiness in
the blood).
Advice to patients
The harmful effects associated with drinking (physical and
psychological damage, accidents, crime and violence, social disorder,
family breakdown, reduced economic production) are well known. These
effects are caused by a combination of intoxication, chronic high intake
and alcohol dependence.
Advice to the public how much they can safely drink must balance the
benefits against these harmful effects.
In countries like United Kingdom and the United States the advice
given is that men should drink less than 21 units/week and women less
than 14 units/week.
One unit is 8 grams of alcohol, approximately equivalent to half a
pint of beer, a small glass of wine or sherry, or a single shot of
spirits in the measures commonly used in reputed pubs.
The origins of these limits are obscure, but they were endorsed in
1980 by medical bodies such as the Royal College of Physicians, the
Royal College of Psychiatrists, and the British Medical Association.
There are problems in specifying quantities.
* The risk associated with consumption varies between individuals.
* Estimates made by drinkers of the amount they have consumed are
inaccurate.
* Some people might see limit as a target for drinking, rather than
ceiling. Although these arguments are valid, following them is to deny
guidance to individuals who seek it, while colluding with heavy drinkers
in finding reasons why they should not decrease their consumption.
Guidance on drinking that specify quantities, therefore is more useful
than guidance that not.
A study done in United Kingdom in 1994 involving 12,321 male doctors
as subjects showed that mortality rises with more than 21 units. The few
studies that have been made of women suggest that for them mortality
rates starts at a lower level 14 units.
It is wrong, however, to base advice on mortality rates alone.
Alcohol is associated with considerable morbidity to the drinker and to
the family, and social problems. The relationship between these harmful
effects and consumption level must be considered when formulating
guidance on low-risk drinking levels. |
