|

Yet another first at the National Hospital Colombo
By Rosanne Koelmeyer Anderson
|

Ranjith Gamage
|
Sri Lanka has recorded yet another feat in its medical history at the
Colombo National Hospital by having successfully performed the first
Endo Vascular Embolisation of Spinal Dural Arterio Venous Fistula
procedure on a patient who was paralyzed waist downwards with bladder
incontinence on Monday.
The forty-nine year-old Ranjith Gamage from Mawanella who was
immobile and could not move or raise his legs was able to sit up, move
and bend his lower limbs without any discomfort by the second day after
the procedure. Ranjith who is now undergoing physiotherapy was overjoyed
at the possibility of his being able to walk once again, sooner or
later.
The condition which is congenial and comes with age causes loss of
muscle power and gradually weakens. In this case the procedure was very
difficult, Dr. Nihal Wijewardena, Consultant Interventional Radiologist
told the Sunday Observer.
The Endovascular procedure, another alternative and much preferred
procedure to that of surgery, was performed with a puncture in the
femoral artery.

Before the procedure |
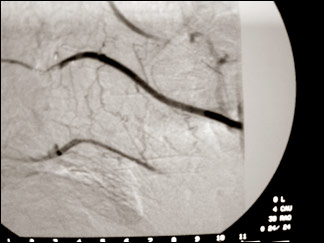
after the procedure |
With the help of a Guiding Catheter, micro catheter and a micro wire
system the abnormal vessel in the spine is accessed and and those
abnormal vessels are blocked using Cynoacrilate glue. Once the abnormal
vessels are filled with this glue the blood flow to the spinal cord was
regulated back to normalcy, Dr. Wijewardena explained.
“Promptly sitting up with a broad smile, Ranjith Gamage said” he was
very relieved now as he was now able to move and bend his lower limbs
quite comfortably making the procedure yet another feat for the doctors
at NHS, Colombo.
“Meanwhile, on the same day yet another rare procedure was done by
Dr. Wijewardena and Dr. Lakmalie Paranahewa with assistance of Prof.
Santhosh Joseph, of Sri Ramachandra Medical School, Chennai and a team
of dedicated anaesthetic doctors headed by Dr. Mrs. Hapuarachchi, and
the neurosurgical team at NHSL on a patient with” a condition of
cerebral aneurism; an Endovascular procedure which although could
performed is not being done due to the simple reason of non availability
“of necessary procedural equipment at the Colombo National Hospital as
the cost ranges per case would cost between” Rs. 500,000 to over 1
million rupees depending on the size of the aneurism. In this case, the
patient was agreeable to bear the cost for the procedure, while the
procedure lasted about 4-5 hours, Dr. Wijewardena said.
“Endovascular procedure for Cerebral aneurism could be done in Sri
Lanka like in other countries. Even the findings by” the “International
Sub Arachnoid” (tm)s Trial (ISAT) conducted recently states that the
Endovascular procedure has proved to be a much preferred procedure than
brain surgery. But, in some instances brain surgery becomes inevitable.
“Endovascular procedure which involves the use of a Guiding catheter,
a micro catheter, a micro guide wire and coils” which are sent after
making a puncture in the groin of a patient. Thereafter, a micro
catheter is introduced through the guiding catheter with the micro wire
in to the aneurism. Coils are then introduced into the aneurism to stop
the blood flow into it. The coils are very costly and “the number of
coils needed depend on the size of the aneurism, Dr. Wijewardena further
explained.”
“There are many patients with cerebral aneurism and it is more common
among the 40-60 age group where the prevalence of degenerative diseases,
Atherosclerosis and vascular diseases are high.
It could be classified as a stress related condition which could be
triggered off any given time. It is uncommon in children. However,
although the risk of rupture is difficult to determine precisely there
is an estimated 1-2 per cent of cerebral aneurism ruptures per year,”
(tm) he added.
“The aneurism raptures and there is haemorrhage then the patient has
to be sorted out within 24 hours: there could be a high risk of re
bleeding  and this could be fatal. Once bleeding has occurred an
estimated 20-50 per cent risk of re bleeding is there within the first
two weeks. Cerebral aneurism” could be detected during an incidental
finding having complained of bouts of severe headache, weakness or loss
of consciousness where initially a CT scan is done. If there is a bleed,
an angiogram is also done to diagnose a cerebral aneurism. In 2007,
three hundred and sixty cerebral angiograms were done at the National
Hospital, Dr. Wijewardena added. Thus, having the necessary equipment at
all given times is of great importance because the condition is most
often life threatening.
However, an important yet unexploited procedure in Sri Lanka due to
the high financial burden for the Ministry of Healthcare and Nutrition,
this has nevertheless proved to be a vital decision and step forward for
medical advancement.
The expertise is available but the equipment for the procedure is
not, thus depriving many patients suffering from cerebral aneurism of
availing themselves of the more plausible alternative, compelling them
to go in for brain surgery.
Breastfeeding - the first 6 months of life
Increasing optimal breastfeeding practices could save an estimated
1.5 million infant lives annually. Up to 55 percent of infant deaths
from diarrhoeal disease and acute respiratory infections may result from
inappropriate feeding practices. Optimal feeding for sustained child
health and growth includes initiation of breastfeeding within the first
hour of life, exclusive breastfeeding for six months, timely
complementary feeding with appropriate foods, and continued
breastfeeding for two years and beyond.
During the first 6 months of life, infants should be
exclusively breastfed. This means that the healthy baby should
receive breastmilk and no other fluids, such as water, teas, juice,
cereal drinks, animal milk or formula.
Exclusively breastfed babies are much less likely to get diarrhoea or
to die from it than are babies who are not breastfed or are partially
breastfed. Breastfeeding also protects against the risk of allergy early
in life, aids in child spacing and provides protection against
infections other than diarrhoea (e.g. pneumonia). Breastfeeding should
be continued until at least 2 years of age.
The best way to establish the practice is to put the baby to the
breast immediately after birth and not to give any other fluids.
Advantages and benefits of breastfeeding are listed below. Some or
all of them may be explained to mothers using simple language.
If breastfeeding is not possible, cow’s milk or milk formula should
be given from a cup.
This is possible even with very young infants. Feeding bottles and
teats should *never* be used because they are very difficult to clean
and easily carry the organisms that cause diarrhoea.
Careful instructions should be given on the correct preparation of
milk formula using water that has been boiled briefly before use.
Advantages and benefits of breastfeeding
1. Saves Lives Currently there are 9 million infant deaths a year.
Breastfeeding saves an estimated 6 million additional deaths from
infectious disease alone.
2. Provides Initial Immunization. Breastmilk, especially the first
milk (colostrum), contains anti-bacterial and anti-viral agents that
protect the infant against disease, especially diarrhoea. These are not
present in animal milk or formula. Breastmilk also aids the development
of the infant’s own immune system.
3. Prevents Diarrhoea Diarrhoea is the leading cause of death among
infants in developing countries. Infants under two months of age who are
not breastfed are 25 times as likely to die of diarrhoea than infants
exclusively breastfed. Continued breastfeeding during diarrhoea reduces
dehydration, severity, duration, and negative nutritional consequences
of diarrhoea.
4. Provides complete and perfect nutrition.
Breastmilk is a perfect food that cannot be duplicated. It is more
easily digested than any substitute, and it actually alters in
composition to meet the changing nutritional needs of the growing
infant. It provides *all* the nutrients and water needed by a healthy
infant during the first 6 months of life. Formula or cow’s milk may be
too dilute (which reduces its nutritional value) or too concentrated (so
that it does not provide enough water), and the proportions of different
nutrients are not ideal.
5. Maximizes a child’s physical and intellectual potential.
Malnutrition among infants up to six months of age can be virtually
eradicated by the practice of exclusive breastfeeding. For young
children beyond six months, breastmilk serves as the nutritional
foundation to promote continued healthful growth. Premature infants fed
breastmilk show higher developmental scores as toddlers and higher IQs
as children than those not fed breastmilk.
6. Promotes the recovery of the sick child.
Breastfeeding provides a nutritious, easily digestible food when a
sick child loses appetite for other foods. When a child is ill or has
diarrhoea, breastfeeding helps prevent dehydration. Frequent
breastfeeding also diminishes the risk of malnutrition and fosters
catch-up growth following illness.
7. Supports food security. Breastmilk provides total food security
for an infant’s first six months. It maximizes food resources, both
because it is naturally renewing, and because food that would otherwise
be fed to an infant can be given to others.
A mother’s milk supply adjusts to demand; only extremely malnourished
mothers have a reduced capacity to breastfeed.
8. Bonds mother and child. Breastfeeding immediately after delivery
encourages the “bonding” of the mother to her infant, which has
important emotional benefits for both and helps to secure the child’s
place within the family. Breastfeeding provides physiological and
psychological benefits for both mother and child.
It creates emotional bonds, and has been known to reduce rates of
infant abandonment.
Silent treatment or poor communication?
Tips before you talk to a doctor:
By Dr. R. A. R. Perera, Consultant Psychologist
These days many doctors are responding to patients demand for better
communication. A doctor cannot be fully competent if they don’t
communicate effectively with their patients.
Far too often the ‘first wake-up call’ comes from a patient who
complains about the medical care they have received. In fact, underlying
many, and perhaps most complaints, is the fact that the doctor failed in
some communication dimension, rather than in some more technical aspect
of the care.
Numerous surveys show the need for more effective doctor-patient
communications even though many physicians excel in this field. Yet,
even as a shortage of physicians is increasing and case loads are
getting heavier, patients are becoming more educated about health
issues. They are demanding better communication between themselves and
their physicians and others in the health-care industry. It’s become a
crucial issue.
Generally, most patients are pretty efficient at telling their own
stories. A doctor being on time to see patients is probably the best way
to keep them happy although this is difficult with urgent calls and
hospital and other commitments.
A physician may miss critical things if the patient is nervous and
don’t really wish to say something about him or her.
Here are few tips on how to get the best from a consultation with
your physician:
* Think about what seems to be wrong. When did it start? What are the
symptoms? How bad is the pain on a scale 1-10.
* Write down brief details on a single page along with medical
history, any medications being taken the dosage and frequency. Give the
page to the doctor and keep a copy for yourself.
* List questions to ask before you arrive for your appointment.
Describe your problem verbally and concisely. If you are too embarrassed
to talk, write it down or hand over a relevant page from a magazine.
* Take someone with you if you feel that’s useful. Write down what
you have been told by your physician as soon as you go home.
* Speak up if there is any examination, procedure or medical jargon
that you do not understand. It is the doctor’s duty to explain to you in
simple language, the problems you have and what he is going to do about
it.
In Sri Lanka some doctors due to lack of time do not perform this,
but it is not an excuse. In countries like England, United States and in
Canada a doctor can be sued for not letting the patient know his or her
problem in simple language where the patient could understand his or her
medical situation.
* If you are sick, or need to talk over something, visit your family
doctor first and get a referral letter, without straight going to a
specialist.
* Make sure that you are informed of the results of any tests, scans
or X-rays, which are done, in your subsequent visit.
* Don’t waste the doctor’s time by telling unnecessary things if you
think it is not relevant to your present medical or psychological
problem, unless the doctor ask about it.
The number I think is that a doctor should treat his patient the way
he (the doctor) liked to be treated if he goes to a physician. A doctor
should be straightforward and clear in discussing a medical situation
and has to show genuine interest in the patient and his family, even
when very busy.
One thing medical schools are stressing more than ever is the need
for doctors to refrain from using medical jargon that patients, might
not understand.
After medical credentials a patient like his or her doctor to have a
sense of humour, the ability and desire to listen, professionalism, a
friendly staff and well kept waiting room, clean fingernails and ability
to apologize for running late and if possible call and tell patients
that their appointments will be delayed.
Breastfeeding
Best for baby Reduces incidence of allergies Economical - no waste
Antibodies - greater immunity to infections Stool inoffensive - never
constipated Temperature always correct and constant Fresh milk - never
goes sour in the breast Emotionally bonding Easy once established
Digested easily within two to three hours Immediately available
Nutritionally balanced Gastroenteritis greatly reduced. |
