|

PD - the commenest movement disorder affects 85%
hospital patients:
Positive attitude, best therapy for Parkinson's disease
By Carol Aloysius
Parkinson's disease, although a common movement disorder affecting a
significant proportion of the elderly population globally and in Sri
Lanka, is still not well understood by the victims or their care givers.
Few are aware of the warning symptoms they must look for so that they
can get early treatment before they progress. Fewer still are
knowledgeable about how the disease can be controlled and the role that
drugs and exercises play in speeding up their recovery.
The Sunday Observer sought the help of Consultant Neurologist Sri
Jayawardenepura Hospital Dr Harsha Gunasekara for answers.
Excerpts ...
Q. How would you describe Parkinson's disease?
A. Parkinson's disease (PD) is a chronic, progressive
neurological disorder which is characterised by pathological damage to
an area of the brain called substantia nigra. This area influences all
voluntary movements of the body.
Q. Is it a common condition worldwide and in Sri Lanka?
A. PD is a relatively common disease in the elderly. It may
affect around two percent of the population over the age of 70 years. On
average, it affects one person in every 1000 of the population. People
as young as 20 have developed PD, but this is rare.
Q. What is the estimated population affected by it in Sri
Lanka? Has there been a national survey?
A. Epidemiological basis of the disease has not been studied
in Sri Lanka. However, in hospital based studies in Sri Lanka, PD has
been the commonest movement disorder affecting 85 percent of patients in
one such study done in Colombo.
Q. Is it limited to certain age groups? Ethnicity? Gender?
Districts?
A. As mentioned earlier, PD predominantly affects people in
their old age. Men are affected more than women (male: female ratio is
3:2).
A lower incidence of the disease is been found in Asians and Africans
compared to the Caucasians.
Q Who are the biggest risk groups, and why?
A. Age is the most important risk factor. Presences of family
history, exposure to certain toxins and head injury are also associated
with increased risk.
 Q.
Although as you say mostly elderly persons are at risk, do you see a
change in the age group with younger people getting the disease? Q.
Although as you say mostly elderly persons are at risk, do you see a
change in the age group with younger people getting the disease?
A. The disease can occur in persons in the younger age groups.
However, it is essential that certain diseases which may mimic PD are
ruled out in younger people before establishing a diagnosis of PD. One
such important disease is Wilson's disease caused by abnormal copper
metabolism and treatable if detected early.
Q. Is it a disease that is inherited?
A. PD in general is not an inherited disease. However, certain
families may be more likely than others to develop the disease because
of an abnormality of their genes. The genetic abnormalities detected are
from different chromosomes and this occurs only in a minority of
patients.
Q. Can any other disease such as Huntington's chorea be
confused with Parkisonism?
A. Yes. As opposed to "classical" PD, "Parkinsonism" refers to
presence of symptoms of the disease (discussed below) in association
with a wide variety of other diseases. Huntington's chorea is one such
disease.
Q. Is it infectious?
A. No. The only relationship of the disease to infection has
been with some types of encephalitis causing "Parkinsonism" at a later
stage rather than causing PD itself.
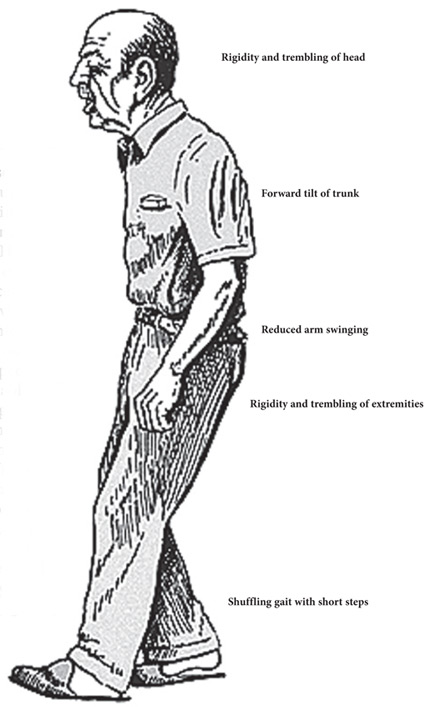
Q. What are the symptoms?
A. The main symptoms of the disease are tremor
(shaking/trembling), stiffness (rigidity), slowness of movement and
problems with posture and balance. Tremor is the commonest symptom and
the initial symptom in many.
It usually affects one side of the body, just one limb or the thumb
alone. It is most noticeable when relaxing and disappears when
performing a task and when sleeping. Stiffness may not be noticed by the
patient. Slowness of movement is most noticeable with walking and
getting up from a chair. Limitations of facial expression, monotonous
speech with excessive drooling of saliva and poor hand writing ("micrographia")
are also associated symptoms. Postural changes are marked by a stoop
forwards and flexed (bent) position of arms and legs. Walking with small
and fast shuffling steps with a tendency to stumble forwards or
backwards are noticeable in a well-established case.
Q. Any other symptoms?
A. In addition to the "motor" symptoms (symptoms associated
with movement) discussed above, the disease can cause a wide range of
"non-motor" symptoms which include pain, problems with sleep, memory,
bladder and bowel control, sexual functions, depression and anxiety.
Q. Can any of these involuntary movements be also seen in
young people and adolescents? e.g. twitching, trembling hands. If so
why?
A. Tremor or trembling is a common symptom and not unique to
PD. An exaggerated physiological tremor may be caused by anxiety states
and with use of certain medications. Essential tremor is a hereditary
disease which can affect young people and can mimic PD. A diagnosis of
PD should be made only after ruling out all these conditions.
Q. Can they be detected early? How long before it progresses
to an advanced state?
A. PD is a progressive neurological disorder and can be
detected early after clinical assessment. It is important to remember
that the changes in the brain would have been happening before the signs
and symptoms of the disease becomes apparent. Progression of the disease
could occur in a similar fashion over a period of few years - more
quickly in some people than in others.
Q. Can early detection arrest the progress of the disease?
A. This concept also known as "Neuroprotection" has been
studied extensively using different medications which have shown
different results. Further research will be needed to establish
definitive neuroprotective drugs.
Q. What are the main causes for the disease?
A. Classical PD has no underlying cause and occurs as a result
of structural changes of a specific area of the brain called substantia
nigra (see diagram).
This in turn results in a reduction of a neurotransmitter chemical
called "dopamine" (neurotransmitters are chemical messengers within the
brain which help the nerve cells to communicate).
Q. Can other factors also bring it on e.g. strong psychiatric
drugs, pre-conditions such as diabetes, cholesterol, and hypertension?
Can NCD's aggravate the condition?
A. These conditions can sometimes cause a "secondary
parkinsonism". Some classes of medications used to treat psychiatric
disorders such as neuroleptics, and some medications used in the
treatment of vomiting and dizziness ("phenothiazines") when used over a
period of time can cause symptoms of PD. Patients should obtain advise
from their respective specialists regarding changing or discontinuing
these medications before doing so.
Conditions such as diabetes, high cholesterol levels and high blood
pressure do not cause PD but will increase the risk of Stroke (a NCD).
Stroke in turn can sometimes cause a form of "secondary parkinsonism"
called "Arterio-sclerotic parkinsonism".
Q. Is Parkisonism curable? Reversible?
A. Some forms of secondary parkinsonism may be reversible, for
example when the causative medication is stopped. However, classical PD
is not so, but can be well controlled with medications.
Q. If a person wants to find out he/she has Parkinson's
disease, how can he set about it? Are there tests such as blood tests,
X-rays or a brain scan?
A. PD has to be diagnosed clinically. Blood tests and a brain
scan (CT or MRI) may be required in some patients to rule out other
disease states.
Q. Where can these tests be done? At an OPD clinic?
A. Yes, if you are worried about any symptoms suggestive of
PD, a clinical assessment and any tests if necessary could be done at an
OPD clinic.
Q. Are they costly, if done in the private hospitals?
A. No, most patients do not need any specific tests for
diagnosis which can be made after a clinical assessment.
Q. Why is a person with Parkinsonism unable to show his
emotions? Does it mean that it reduces the emotional as well as physical
movements?
A. This is due to the loss of facial expression caused by
slowness of movement affecting the muscles of facial expression.
The patient may look sad or depressed with reduced blinking, and may
appear to stare and may not appear to smile or laugh as before.
Q. What is the Western treatment? Drugs? Shock treatment?
A. Patients with classical PD can be well controlled on
medications. The basis for drug therapy is to counteract the reduction
of the neurotransmitter "dopamine" in the affected area of the brain.
Additional medications may be needed to control certain non-motor
symptoms discussed above. Patients should adhere to medical advice
during their treatment and medications should never be stopped abruptly.
Shock treatment is used in severe depression and has no role in PD.
Q. What about alternate treatment such as acupuncture and
physiotherapy? Can they help?
A. As with many other diseases, complimentary therapies such
as acupuncture may have their place along with standard treatment.
Q. What role do physical exercises play?
A. Exercise plays an important part in any healthy lifestyle.
Exercises help in reducing symptoms of PD, especially stiffness and also
improve mobility, posture, balance and gait. In general, Aerobic
exercise increases oxygen delivery and neurotransmitters to keep our
heart, lungs, and brain healthy and also reduce depression.
Q. Do they need supervision?
A. Physiotherapists will advise on exercise routines which
then could be followed at home.
They will also give advice on moving around at home more easily and
getting into and out of bed and bath etc. Having Parkinson's Disease
should not stop you from taking part in any of your usual exercise
routine, and it's a good idea to continue for as long as possible.
Q. What kind of physical exercises can you recommend to reduce
the tremors - e.g. walking, climbing steps, dancing, carrying a
newspaper?
A. Exercises can be targeted in improving all the symptoms
rather than tremor alone. Exercises that require large, rhythmical
movements through a full range of motion have been shown to decrease
rigidity (e.g. aerobic exercise using music).
Touching the limb that is shaking to quieten the movement and
activities to reduce stress levels will help minimise tremor.
Q. Are there any recent developments in medical science to
treat this disease?
A. Newer medical therapies such as using new neuroprotective
drugs and new formulations of existing medications are being used in
some countries which have shown benefits. Surgical therapies, deep brain
stimulation techniques and Radiosurgery offer help for patients with
poor response to medical treatment but only after careful selection.
Q. What about stem cell treatment? I'm told that some of stem
cells treatments have had a very significant impact on reducing tremors
in a few countries where it is being done. Your comments?
A. Stem cells are 'unspecialised' cells which can develop into
almost any cell in the body.
Researchers are investigating stem cells in the hope that they could
be used to grow nerve cells to replace those lost in the brain affected
by PD. Studies on stem cells are still at an early stage and, as yet, no
appropriate clinical trials have been carried out. Only when stem cells
have been thoroughly tested and proven to be safe will they become
available to patients with Parkinson's disease.
Q. Does diet play a role? If so, what foods should be eaten
and what should be avoided?
A. Although there is no special diet for people with
Parkinson's disease, eating a well-balanced, nutritious diet is
extremely beneficial.
Q. Your message to the public?
A. Establishing a correct diagnosis is essential before
starting treatment with medication.
Once diagnosis is established, it's probably the hardest thing anyone
will ask you to do, but try to accept your disease. It's a good idea to
learn about the disorder and work with the professionals to help control
your symptoms best. Your own positive attitude is the best therapy. PD
is one area where intensive research is taking place to develop new
treatments that will slow or even reverse the disease in the future.
Carrying extra weight can be healthier for older people
Older people with a BMI(body mass index) in the overweight range live
longer, according to the results of a new study.
Deakin University's professor of nutrition and ageing, Caryl Nowson,
led a research team that looked at the relationship between BMI and risk
of death in people aged 65 years and older. They found that the lowest
risk of death was among those with a BMI
 of
around 27.5, which is considered overweight according to the World
Health Organisation (WHO) guidelines; and mortality was significantly
increased in those with a BMI between 22 and 23, which is in the normal
weight range. The results of the study, suggest that current BMI
recommendations may not be suitable for older adults. of
around 27.5, which is considered overweight according to the World
Health Organisation (WHO) guidelines; and mortality was significantly
increased in those with a BMI between 22 and 23, which is in the normal
weight range. The results of the study, suggest that current BMI
recommendations may not be suitable for older adults.
"It is time to reassess the healthy weight guidelines for older
people," Prof Nowson said.
"Our results showed that those over the age of 65 with a BMI of
between 23 and 33 lived longer, indicating that the ideal body
weight for older people is significantly higher than the recommended
18.5 - 25 'normal' healthy weight range."
For this project the research team reviewed studies published between
1990 and 2013 that reported on BMI and risk of death in people aged 65
years and over, collectively these studies followed around 200,000
people over an average of 12 years.
The results showed the following connection between BMI and risk of
death:
-12 percent increased risk when BMI was 21-22 (which is within the
healthy weight range)
-19 percent increased risk when BMI was 20-20.9 (which is still
within the normal range)
-8 percent increased risk for BMI 33-33.9 (in the obese range)
Prof Nowson suggests that most older people need to get off the
weight loss bandwagon.
"These findings indicate that, by current standards, being overweight
is not associated with an increased risk of dying," Professor Nowson
said. "Rather it is those sitting at the lower end of the normal range
that need to be monitored, as older people with BMIs less than 23 are at
increased risk of dying."
Advice on ideal body weight should take into account factors other
than BMI, Prof Nowson said.
"Factors such as chronic diseases and the ability to move around need
to be considered as there is no real issue with being in the overweight
range unless it is preventing people from moving around freely," she
said.
"Rather than focussing on weight loss, older people should put their
efforts into having a balanced diet, eating when hungry and keeping
active.
"Putting too much emphasis on dietary restrictions also increases the
risk malnutrition in this age group. Malnutrition in older people is not
well recognised as this can occur even when BMI is in the overweight
range."
- MNT
|

