|

World Psoriasis Day on October 29:
Psoriasis, a common chronic skin controllable ailment
Beware of quacks claiming miracle cures:
By Carol Aloysius
Hot humid climates, poverty, poor sanitation and under nutrition have
contributed to a rise in skin ailments mostly in developing nations.
Psoriasis is one of them. While there is no national data on its
incidence, published records from patients attending government clinics
in certain districts such as Galle, Kandy, Matara and Polonnaruwa reveal
that 3.5-7 percent of such patients suffer from psoriasis.
 The often visible disfiguring marks and scars left by the disease on
their skin, has had a psychological impact on the sufferers. So much so
that many voluntary groups including the National Psoriaris Foundation,
USA organises world wide events to raise funds to improve the quality of
lives of those affected by the disease, on World Psoriasis Day which
falls on October 29. The often visible disfiguring marks and scars left by the disease on
their skin, has had a psychological impact on the sufferers. So much so
that many voluntary groups including the National Psoriaris Foundation,
USA organises world wide events to raise funds to improve the quality of
lives of those affected by the disease, on World Psoriasis Day which
falls on October 29.
Psoriasis is a chromic skin ailment which can be controlled with the
right medication. It is not infectious and those who have it should in
no way be embarassed or isolate themselves from society. Nor should they
seek help from unqualified physicians claiming to have miracle cures for
this chronic infection, as such treatments could undermine their health
and damage their body organs including the liver, warns an eminent
Dermatologist.
Dr Mrs INDIRA KAHAWITA, Secretary, College of Dermatologist, and
Consultant Dermatologist at the Karawanella Base Hospital, discusses
some of the symptoms and treatment procedures for this disease with the
Sunday Observer.
Excerpts...
Q. Skin diseases are common all over the world but some are
more common in this part of the world. What are they and why?
A. It is widely believed that infections of the skin are
commoner in this part of the world compared to the west. But the
incidence of infections seems to have gone down with better living
conditions.
Q. What are the commonest skin diseases in Sri Lanka? Does our
humid climate cause certain of these ailments?
A. The commonest skin problem among clinic attendees in Sri
Lanka is eczema. The other common conditions are viral and fungal
infections, psoriasis acne and problems related to pigmentation. Our
humid climate may contribute to certain problems like fungal infections.
Q. Is Psoriasis (Pothu kabara) one of them?
A. Yes, psoriasis is one of the common skin problems in
persons attending skin clinics.
Q. How many people have this condition in our country? Are
there hospital records to indicate a rough estimate of people visiting
hospital for treatment of psoriasis?
A. There are no accurate records of the numbers affected as no
studies on prevalence of skin diseases in Sri Lanka have been
undertaken. But published reports from Galle, Kandy, Matara and
Polonnaruwa reveal that 3.5 - 7 percent of persons attending skin
clinics are suffering from psoriasis.
Q. How is psoriasis described in medical terms?
A. Psoriasis is an inflammatory disease affecting the skin,
hair, nails and the joints.
Q. Is it a chronic disease or does it only last temporarily?
A. It is a chronic disease. A person may achieve complete
clearance of skin lesions during an episode but the disease may recur
sometime later.
|

A patient with psoriasis on the back |
Q. Is it infectious?
A. No.
Q. What causes it?
A. The exact cause for psoriasis is not known. But heredity
may play a role. A persons has a 10 percent risk of developing psoriasis
if a parent is affected. This risk nears 50 percent if both parents are
affected. The genetic transmission is very complex and psoriasis is
considered to be due to a combination of heredity and the environment. A
family history of Psoriasis is found in 30 percent of those infected.
Q. Does an internal disorder have anything to do with it?
A. Psoriasis is now considered as a metabolic disease, which
means it is not just a skin disease but a disease affecting other
systems in the body.
Q. Is it an allergy? Can certain foods bring it on?
A. It is not an allergy. Usually foods cannot cause psoriasis
but a food allergy may precipitate an episode.
The other things that may precipitate an episode are infections,
climatic changes, hormonal changes, mental and physical stress and
trauma to the skin.
Certain drugs used in treatment of high blood pressure and malaria
may cause a recurrence.
Q. Who are those most at risk of getting it?
A. There are no specific "at risk" groups except perhaps those
with a family history of psoriasis. Both sexes are equally affected and
those in the 2nd and 3rd decades and 6th and 7th decades are more
vulnerable.
Q. Can children and babies get it?
A Children and even babies may get it but it less common than in
young adults and adults.
Q. What are the symptoms 1) at the early onset of the disease
2) advanced stage?
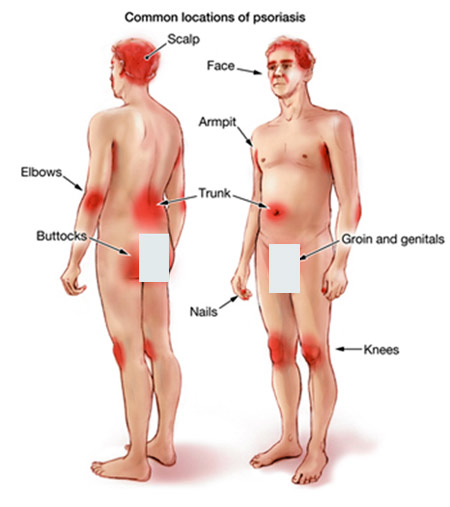
A. The commonest feature is the red to pigmented scaly
circular raised lesion with slivery scales on it. These may occur
anywhere in the body but commoner in the back, front of chest, back of
arms and forearms and the shins.
There may be excessive scaling of the scalp, which may occur before
the skin lesions become evident.
With advancing disease the nails may get destroyed with
discolouration and separation of the nail from the nail bed.
In later stages there may peeling off of skin of the whole body or
formation of small pustules around the skin lesions.
Q. Is it treatable if detected early?
A. Psoriasis is treatable at any stage. But early treatment
ensures better results.
Q. If cured can the infection re-emerge later?
A. Complete clearance may be achieved but the disease is
likely to re-emerge later.
Q. Are there other health complications that can arise from
it?
A. Psoriasis is now considered to be a disease affecting the
other organs of the body too. There is an increased risk of diabetes and
heart attacks in persons who are suffering from psoriasis. But the good
thing is this risk gets reduced if the psoriasis is well under control.
Q. Is it correct that it can cause arthritis joint pain and
swelling?
A. Yes, arthritis is a well known complication of psoriasis.
It may involve any type of joint including the large joints, the small
joints of the hands and feet and the back.
Q. How do you treat it? With drugs? heat?
A. There are many treatment modalities.
The major groups are local applications (creams, ointments, balms,
lotions and pommades for the scalp) systemic drugs (tablets and
injections) and light therapy (ultra violet light)
Q. What are the most recent advances in treatment? Are they
available here?
A. the recent advances include ultraviolet light therapy and
newer medications like drugs that modify the immune response (biologic
therapy) UV therapy and some biologics are available in SL.
Q. Is laser treatment used for psoriasis.
A. Laser therapy is usually not used in psoriasis.
Q. Is treatment free in state hospitals? Are there special
units for treating these patients?
A. Most treatments available free in state hospitals. All skin
clinics are geared to treat patients with psoriasis but the facilities
available may vary between hospitals.
Q. Is home medication possible? How?
A. Most patients are treated as out-patients with the
medications for a month or two weeks being provided during a clinic
visit. Some may need hospitalisation if they develop complications.
Q. Psoriasis is sometimes confused with certain other skin
diseases such as eczema and urticaria. What is the difference?
A. Psoriasis may be confused with eczema and dandruff. But
lesions of psoriasis show excessive scaling and bleeding points when the
scale is removed by scratching.
Q. Any Do's and Don'ts for avoiding the diseases and treating
it?
A.Seek treatment early. Follow instructions given at the clinic when
taking the medications Follow treatment for the specified period of time
Have a healthy diet. Proteins are essential to regenerate the damaged
skin hence a good intake in the diet is necessary.
Cut down on sugar and fats.Avoid alcohol and smoking. Try to avoid
trauma to the skin as the lesions may appear in sites of trauma
Q. Your advice to patients and to the public in general?
A. Psoriasis is a disease which can be controlled very well.
There is no need to shy away from society of you have psoriasis.
Many individuals in important positions in society including doctors
have been affected by psoriasis but the disease has not prevented them
from becoming successes in life. You may be affected by a chronic
disease but there is help available free of charge at the nearest skin
clinic.
The other message is not to get misled by unqualified persons who
claim that they can cure you of psoriasis.
Taking some unknown medications may lead to permanent damage to
organs including the liver.
Facts on psoriasis
Psoriasis is a skin condition that causes red, flaky, crusty patches
of skin covered with silvery scales. These patches normally appear on
your elbows, knees, scalp and lower back but can appear anywhere on your
body. Most people are only affected in small patches. In some cases, the
patches can be itchy or sore. Psoriasis affects around 2 percent of
people in the UK. It can start at any age, but most often develops in
adults under 35 years old. The condition affects men and women equally.
The severity of psoriasis varies greatly from person to person. For
some people, it is just a minor irritation, for others it has a major
impact on their quality of life. Psoriasis is a long-lasting (chronic)
disease that usually involves periods when you have no symptoms or mild
symptoms, followed by periods when symptoms are more severe. When to
seek medical advice
You should see your GP if you think you may have psoriasis. They can
often diagnose the condition based on the appearance of your skin.
Why it happens
Psoriasis occurs when the process by which the body produces skin
cells is accelerated.Skin cells are normally made and replaced every
three to four weeks, but in psoriasis this process only lasts about
three to seven days.The resulting build-up of skin cells is what creates
the patches associated with psoriasis.
Although the process is not fully understood, it is thought the
increased production of skin cells is related to a problem with the
immune system.The immune system is your body's defence against disease
and infection, but in people with psoriasis it attacks healthy skin
cells by mistake. As psoriasis can run in families, there is also
thought to be a genetic element to psoriasis. However, the exact role
that genetics plays in causing psoriasis is unclear.
Many people's psoriasis symptoms start or become worse because of a
certain event, known as a trigger. Possible triggers of psoriasis
include an injury to your skin, throat infections and using certain
medicines. The condition is not contagious so it cannot be spread from
person to person.
Treating psoriasis
There is no cure for psoriasis, but a range of treatments can improve
symptoms and the appearance of the affected skin patches.
In most cases, the first treatment used will be a topical treatment,
such as vitamin D analogues or topical corticosteroids. Topical
treatments are creams and ointments applied to the skin. If these are
ineffective or your condition is more severe, a treatment called
photo-therapy may be used. Photo-therapy involves exposing your skin to
certain types of ultraviolet light. In the most severe cases where other
treatments are ineffective, systemic treatments may be used. These are
oral or injected medicines that work throughout the whole body. Find out
more about treating psoriasis.
Living with psoriasis
Although psoriasis is just a minor irritation for some people, the
condition can sometimes have a significant impact on your life.
For example, some people with psoriasis have low-self esteem due to
the affect the condition can have on your physical appearance. It is
also quite common for someone with psoriasis to develop tenderness, pain
and swelling in the joints and connective tissue.
This is known as psoriatic arthritis.Speak to your GP or healthcare
team if you have psoriasis and you have any concerns about your physical
and mental well-being.
They can offer advice and further treatment if necessary. There are
also a number of support groups for people with psoriasis, where you can
speak to other people with the condition.
(from National Health Service,UK)
Siblings of children with autism can show signs at 18 months
About 20 percent of younger siblings of children with Autism Spectrum
Disorder (ASD) will develop the condition by age 3. A new study has
found that 57 percent of these younger siblings who later develop the
condition already showed symptoms at age 18 months.
 Published in American Academy of Child & Adolescent Psychiatry, this
is the first large-scale, multi-site study aimed at identifying specific
social-communicative behaviors that distinguish infants with ASD from
their typically and atypically developing high-risk peers as early as 18
months of age. Published in American Academy of Child & Adolescent Psychiatry, this
is the first large-scale, multi-site study aimed at identifying specific
social-communicative behaviors that distinguish infants with ASD from
their typically and atypically developing high-risk peers as early as 18
months of age.
"While the majority of siblings of children with ASD will not develop
the condition themselves, for those who do, one of the key priorities is
finding more effective ways of identifying and treating them as early as
possible," said lead author Katarzyna Chawarska.
"Our study reinforces the need for repeated diagnostic screening in
the first three years of life to identify individual cases of ASD as
soon as behavioral symptoms are apparent."
Chawarska and her co-authors pooled data from eight sites
participating in the Autism Speaks Baby Siblings Research Consortium.
The team closely examined social, communicative, and repetitive
behaviors in 719 infants when they were 18 months old.
The team looked for patterns that might predict a later diagnosis of
ASD. They then followed up when the participants were age three.
"Our research suggests that approximately half of the siblings who
are later diagnosed with ASD display signs suggestive of ASD at 18
months, and in those who appeared asymptomatic at 18 months, symptoms
appeared between 18 and 36 months," said Chawarska.
Chawarska said what was most interesting to the research team was
that different patterns of behaviors at 18 months may be predictive of
ASD later on. In about 50 percent of siblings, a combination of poor eye
contact and lack of communicative gestures or imaginative play is most
strongly associated with later ASD diagnosis.
In a small percentage of those later diagnosed with ASD, eye contact
may be relatively normal, but they begin to display early signs of
repetitive behaviors and have limited non-verbal communication skills.
"So not only do the behavioral symptoms appear at different ages, but
different combinations of early symptoms may predict the diagnostic
outcome," Chawarska added.
"Linking these developmental dynamics with underlying neurobiology
may advance our understanding of causes of ASD and further efforts to
personalize treatment for ASD by tailoring it to specific clinical
profiles and their developmental dynamics."
- MNT |

