|

November 12 is World Pneumonia Day :
Pneumonia - early detection and treatment, the key
By Carol Aloysius
Pneumonia kills millions of persons especially children under five as
well as elderly persons with low immune systems every year. The WHO and
UNICEF have repeatedly reiterated that unless this killer disease is
drastically reduced or eliminated millions of young children may not
live to celebrate their fifth birthday. Surveys have shown that in 2011
alone, 1.3 million young children across the world died from
complications resulting from developing pneumonia.
Yet, these deaths, like most other preventable deaths which occur in
developing nations are preventable with early detection and early
intervention.
|
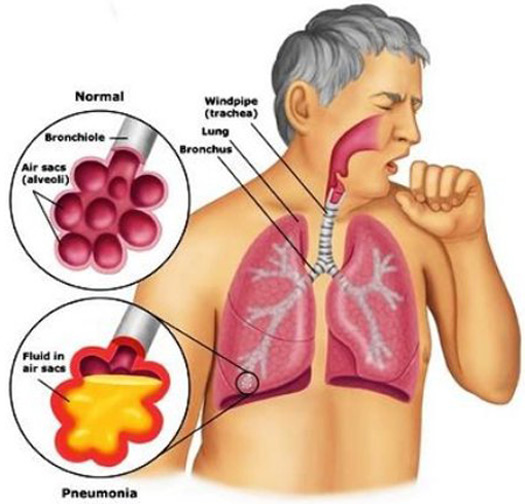
Persistent coughing can be a symptom of pneumonia |
What prevents early and proper treatment of pneumonia is often
closely linked to ignorance on the part of mothers and carers among
other reasons.
President, Sri Lanka College of Pulmonologists, Consultant
Respiratory Physician, National Hospital for Respiratory Diseases,
Welisara, Dr SAMAN KULARATNE tells readers more about this disease and
how it can be prevented in his interview with the Sunday Observer.
Excerpts...
Q. On November 12 the world will be observing Pneumonia Day.
Pneumonia is a subject that not many people know about. What is
pneumonia? How do you describe it in medical terms?
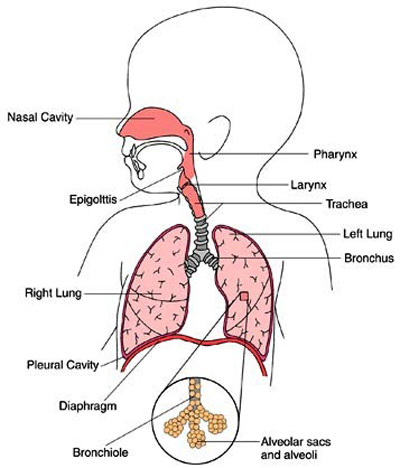
A. Pneumonia is an infection of the lungs. This disease is
characterised by inflammation of the lungs primarily affecting the air
sacs known as alveoli.
Q. Is it a virus or bacteria or both?
A. It is usually caused by infection with viruses or bacteria
and rarely by other organisms such as fungi.
Inhalation of chemical irritants, certain drugs and other conditions
such as autoimmune diseases also can cause inflammation of the lungs.
Q. Is it inherited? Is it gender related?
A. Pneumonia is not an inherited disease, but certain
inherited diseases which affect the normal immune system of the body may
predispose to pneumonia and therefore may present with repeated episodes
of pneumonia.
Q. Is it infectious?
A. Yes. Some of the viruses and bacteria causing pneumonia are
highly infectious.
Different routes
Q. How is it transmitted? From the air? Mucous? Food?
A. The viruses may reach the lungs by a number of different
routes. Some viruses are typically contracted when people touch
contaminated objects and then touch their eyes or nose. Other viral
infections occur when contaminated airborne droplets are inhaled through
the mouth or nose. Ones in the upper airway, the viruses may make their
way in the lungs, where they invade the cells lining the airways and
alveoli. Some viruses may reach the lungs via the blood.
Most bacteria enter the lungs via small aspirations of organisms
residing in the throat or nose. Half of the normal people have these
small aspirations during sleep. While the throat always contains
bacteria, potentially infectious ones reside there only at certain times
and certain conditions. Some bacteria such as bacterium that causes
Tuberculosis reach the lungs via contaminated airborne droplets.
Bacteria can spread also via the blood.
Q. Who are those most vulnerable to the disease - infants?
Young children under 5? Adolescents? Elderly?
A. People most at risk are older than 65 or younger than 2
years of age.
Q. Any other risk groups?
A. Other high risk groups include smokers; those who are
malnourished due to health conditions or lack of access to nutritious
foods; those who have underlying lung diseases such as asthma, or
chronic obstructive pulmonary disease; those who have other medical
problems including diabetes, or heart disease.
People who have difficulty in coughing due to stroke, sedating drugs
or alcohol, or have limited mobility are also at risk.
Q. Those with lung infections with viral infections and
underlying impaired body immunity?
A. Those who have had recent viral upper respiratory tract
infections including influenza, and those who have weakened immune
system due to HIV, organ transplant, chemotherapy (for cancer patients),
or chronic steroid (Prednisolone) use are also at risk.
Q. Are there different forms of pneumonia?
A. Doctors use different terms to describe different forms of
pneumonia depending on the distribution of the disease within the lungs,
possible etiological agents and the possible source of infection.
When the infection is confined to one or few of the lobes of the
lungs, this is described as lobar pneumonia. (Right lung has three lobes
and left has two lobes). The term bronchopneumonia is used when the
infection is distributed around the bronchi (small breathing tubes)
without the lobar pattern.
Health facility
Q. How do you describe pneumonia contracted in a hospital
setting and pneumonia acquired outside the health facility?
A. Hospital acquired pneumonia refers to any pneumonia
contracted by a patient in a hospital at least 48 - 72 hours after being
admitted. It is usually caused by bacteria. Community acquired pneumonia
refers to pneumonia acquired outside of hospitals or extended-care
facility.
Q. What are the general symptoms of the disease?
 A. Symptoms of pneumonia can vary from mild to severe. These
include high fever, shaking chills, a cough with phlegm that doesn't
improve or gets worse, shortness of breath with normal daily activities,
and chest pain when you breathe. A. Symptoms of pneumonia can vary from mild to severe. These
include high fever, shaking chills, a cough with phlegm that doesn't
improve or gets worse, shortness of breath with normal daily activities,
and chest pain when you breathe.
Q. Are the symptoms the same in young and old alike?
A. Elderly patients with pneumonia may present with altered
behaviour or confusion.
Q. Can these symptoms be confused with flu at their onset?
A. Yes. Flu also can have some of the symptoms of pneumonia
and flu can also predispose to bacterial pneumonia. So anyone who feels
suddenly worse after a cold or the flu should seek medical advice.
Q. How is pneumonia treated?
A. Suspected bacterial pneumonias are treated with antibiotics
just after assessing the severity of the illness. Doctors assess the
pulse rate, respiratory rate, temperature, oxygen level in the blood and
other parameters in hospitalised patients.
Certain blood, urine and sputum tests are performed to find out the
severity, presence of underlying illnesses such as diabetes, kidney or
liver problems. These tests also help the doctors to find out the exact
organism / germ which is causing the infection. Presence of pneumonia
and the extend of distribution can be assessed by obtaining a chest
X-ray. Possible viral pneumonias are treated with anti viral therapy and
fungal infections with anti fungal treatment. Close monitoring of the
patient and hydration is very important. Some patients with breathing
difficulty may need ICU care and assisted ventilation with the help of
an artificial breathing machine.
Q. Are they available here? Where?
A. All the facilities to treat an ill pneumonic patient are
available in all the major hospitals throughout the country.
Q. Are poverty, living in unsanitary overcrowded areas,
exposure to dust, contributory factors?
A. Yes. Poverty is associated with poor nutrition which is a
well known factor for pneumonia. Airborne infections are known to spread
rapidly in overcrowded areas. The best example is Tuberculosis.
Tuberculosis is common in our urban population with poor housing
conditions. In some occasions we see several cases of pneumonia due to
Tuberculosis within the same area. Exposure to dust is known to cause
various lung diseases which again could predispose to pneumonia.
Q. Do all patients have to be hospitalized under expert
medical management?
A. No. All patients with pneumonia do not need inward
treatment. The doctor can carefully assess the severity of the disease
and decide to treat as an outpatient if the condition of the patient is
stable.
Q. What about home management in the case of less serious
cases? Are there any golden rules to follow?
A. Patients who are being managed at home should take the
medicine prescribed doses regularly for given period and should not stop
half way when they feel better. Maintaining a good fluid intake and rest
at home are very important. One should meet the doctor again or should
get admitted to a hospital if they develop any new symptoms such as
breathing difficulty, bringing up of blood in sputum, feeling not well
with the treatment, chest pain and persistent fever. Those who feel
better should also meet the doctor as advised.
Health complications
Q. Are there other health complications arising from
pneumonia?
A. Yes. Although pneumonia can be treated successfully, some
patients can develop complications. Fluid can get accumulated between
the covering of the lungs (pleura) and the inner lining of the chest
wall; this is called a pleural effusion.
Doctors may aspirate this fluid for analysis and if there is evidence
of infection (called emphysema) a chest tube may be needed to drain the
fluid.
In some patients you may see collection of pus in the area infected
with pneumonia (lung abscess). Lung abscess can usually be treated with
antibiotics; rarely surgical intervention is needed.
Q. What is Septicemia in relation to pneumonia? Is it a
serious condition?
A. Some patients with severe pneumonia can spread the
infection from the lungs to the blood stream. This is known as
Septicemia and carries a very high mortality rate. Patents with evidence
of septicemia and who have breathing difficulty may need admission to
intensive care unit. Some of these patients may also need assisted
ventilation with a help of a breathing machine.
Q. What is the prognosis for patients who have been treated
early?
A. Most patients recover from pneumonia with appropriate
treatment. Mortality rates for inward patients could be high as 10
percent and 30 percent for patients with severe infection requiring
admission to an intensive care unit.
Q. Can the disease be prevented? How? With vaccines?
Prophylactic antibiotics?
A. Yes. There are vaccines to prevent pneumonia. These include
influenza vaccines, pneumococcal vaccine and Hib vaccine. These vaccines
are indicated for those who are at risk of developing pneumonia due to
these organisms especially for elderly people and those who have chronic
lung diseases and heart diseases.
Q. Are these vaccines available in our country?
A. Most of these vaccines are available in Sri Lanka.
Q. What are the risks of having pneumonia for a patient with a
non communicable disease such as cancer, diabetes, hypertension, heart
problems? Will pneumonia aggravate these predisposed conditions and
eventually lead to early death?
A. Pneumonia may result in worsening of underlying chronic
conditions such as heart problems, asthma, chronic obstructive lung
disease. Pneumonia is a common cause of death in cancer patients. It
also may affect the blood sugar levels in diabetic patients. Some
diabetic patients with pneumonia may present with very high or very low
sugar levels.
Lasting health
Q. Are there lasting health implications if a person gets
pneumonia?
A. Yes. Some patients with severe pneumonia may develop
permanent lung damage due to scarring. These patients may later develop
breathing difficulties and can also present with recurrent chest
infections.
Q. What is your message to the public on how to prevent
pneumonia?
A. Infection control measures can help prevent the spread of
pneumonia. Simple practices such as frequent hand washing with soap and
water or alcohol-based hand rub can be effective.
Because pneumonia is spread by contact with infected respiratory
secretions, people with pneumonia should limit face-to-face contact with
uninfected family and friends. Mouth and nose should be covered while
coughing or sneezing, and tissues should be disposed of immediately.
Giving up smoking completely is another important way to prevent
pneumonia. Strict control of diabetes is also important.
Vaccines also play an important role in the prevention of pneumonia
in vulnerable groups especially in people older than 65 yrs and children
below 5 yrs and also in those who have chronic lung and heart diseases.
Sri Lanka free from malaria for two years
 International malaria experts gathered in Colombo to recognise the
country's remarkable achievement and to sign the Colombo Declaration on
Eliminating Malaria International malaria experts gathered in Colombo to recognise the
country's remarkable achievement and to sign the Colombo Declaration on
Eliminating Malaria
Sri Lanka has not reported a local case of malaria since October
2012. If it can remain malaria-free for one more year, the country will
be eligible to apply to the World Health Organization for malaria-free
certification. In 2000, Sri Lanka had over 100,000 cases of malaria.
The Malaria Elimination Group, an independent international advisory
group on malaria elimination, gathered in Colombo for its ninth meeting
to celebrate Sri Lanka's achievements.
At the end of deliberations, the Group signed the Colombo Declaration
on Eliminating Malaria to affirm continued assistance to Sri Lanka.
Following implementation of intensive malaria control measures
between 1946 and 1963, Sri Lanka succeeded in virtually eliminating
malaria from the country. Malaria became invisible to Sri Lanka's
communities, politicians and national leaders. Unfortunately, with only
a few cases left and competing development and health priorities, the
country did not sustain the Anti-Malaria Program in the 1960s. The
consequence was disastrous - Sri Lanka suffered a deadly malaria
resurgence, going from 17 cases in 1963 to over half a million cases in
1969.
The Malaria Elimination Group meeting highlighted the crossroads that
Sri Lanka is at once again: deciding whether to maintain adequate
resources and vigilance to achieve and sustain malaria freedom, or to
risk a second resurgence by losing focus on the benefits of the
prevention of malaria re-introduction.
 Sir Richard Feachem, chair of the Malaria Elimination Group and
director of the UCSF Global Health Group, underscored the main theme of
the Colombo Declaration on Eliminating Malaria and the importance of
maintaining the gains made in Sri Lanka, "I am honoured and proud that,
for the first time in my life, I am visiting a malaria-free Sri Lanka.
This is a huge achievement, and the Ministry of Health and Anti-Malaria
Campaign are to be congratulated. Representatives from 17 countries have
travelled to learn from Sri Lanka's success. Sir Richard Feachem, chair of the Malaria Elimination Group and
director of the UCSF Global Health Group, underscored the main theme of
the Colombo Declaration on Eliminating Malaria and the importance of
maintaining the gains made in Sri Lanka, "I am honoured and proud that,
for the first time in my life, I am visiting a malaria-free Sri Lanka.
This is a huge achievement, and the Ministry of Health and Anti-Malaria
Campaign are to be congratulated. Representatives from 17 countries have
travelled to learn from Sri Lanka's success.
But there is still work ahead: although local transmission of malaria
has ended, Sri Lanka continues to face a serious risk of re-importation
from neighbouring countries.
It is critical that the government sustain its human and financial
investments in malaria elimination - including a robust surveillance
system - to hold the line and keep the country free of the disease."
Today, the threat of re-emergence of malaria in Sri Lanka is driven
by travellers - both Sri Lankan nationals and foreigners - who carry the
disease after being in other malaria-ridden countries. Strong
surveillance systems, multi-sector engagement and rapid follow-up and
response on every imported case will be critical to ensure that these
isolated infections do not spread. The Malaria Elimination Group meeting
and the Colombo Declaration on Eliminating Malaria underscore that with
strong vigilance and commitment, Sri Lanka can safeguard its malaria
achievements and create a healthier, united and economically successful
future. |

