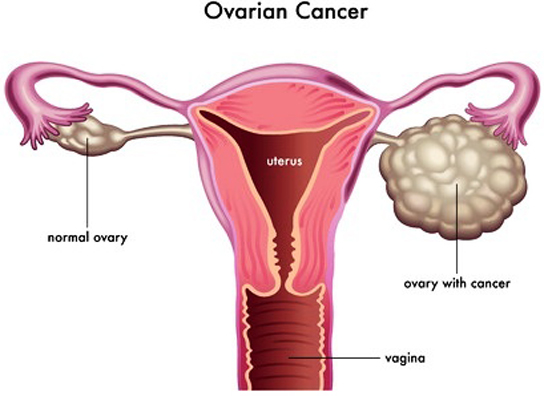
Scientists map the spread of deadliest ovarian cancer
Researchers are providing critical insight into the invasive spread of the most
malignant form of ovarian cancer in a landmark study, published in Nature
Genetics. This is a first in mapping two distinct patterns of ovarian cancer
cell migration in high grade serous ovarian cancer.
The discovery, led by Dr. Sohrab Shah, senior scientist at the BC Cancer Agency,
Associate Professor at the University of British Columbia, and Canada Research
Chair in Computational Cancer Genomics, was made possible through genomic
sequencing techniques and novel software developed by his bioinformatics team at
the BC Cancer Agency.
Tumour
The study was simultaneously published in Nature Methods. The scientists have
answered key unknowns about how deadly ovarian cancers spread, and the
composition of the cancer cell groups that have taken up residence within the
patient’s abdomen.
The study reveals that many cancer cell types make up a patient’s tumour. This
could explain why some cells are susceptible to treatment when others are
resistant, leading to relapse. Also, cell type migration patterns from ovary to
other abdominal sites identified that specific ovary sites contained many more
cell types relative to others.
 These regions could pinpoint ‘gateways’ of cell migration to other abdominal
sites. These regions could pinpoint ‘gateways’ of cell migration to other abdominal
sites.
More than 300 women are diagnosed with ovarian cancer each year in BC, and 80
per cent of women diagnosed with a high grade serous ovarian cancer relapse,
despite an initial response to treatment.
Migration
Unlike most cancers that spread through the blood stream or lymph system, this
study shows that high grade serous ovarian cancer cells have a unique
opportunity to spread prolifically throughout the abdomen.
In mapping the cell migration, Dr. Shah’s team shows how cells are able to
settle and thrive in specific regions of the body causing widespread,
life-threatening disease.
The migration maps were primarily determined in pre-treatment samples with one
exception. Shah’s team studied one patient with multiple relapse specimens.
Notably, only a subset of cancer cells present at diagnosis led to treatment
resistance.
Next steps are to use the innovative techniques developed for this study to
define cell migration maps from additional patients over time with a specific
focus on determining which cells are resistant to treatment. This will allow
researchers to build predictive tools to better inform future care.
This new understanding of how high grade serous ovarian cancer cells migrate
within the patient’s body provides insight that could inform future treatment
selection.
These results indicate that some cancer cells may have had pre-existing
properties of resistance prior to the patient taking any treatment.
This could indicate that a patient requires a much more aggressive,
multi-treatment approach from the start to prevent relapse.
This work is supported by the BC Cancer Foundation through the generosity of
donors from across BC who are committed to improving cancer outcomes for those
impacted by ovarian cancer.
- MNT |

