|
Diabetes:
How much do you know?
By Dr. Indu WAIDYATILAKA
Continued from last week
How is diabetes treated?
Specific treatment for diabetes will be determined by your doctor
based on your medical history, family history, your age, overall health,
the type of diabetes you have, the complications if there are any, your
tolerance for specific medications and your opinion or preference.
Treatment can be discussed under the following headings 1. Diet
control 2. Exercise 3.Oral hypoglycaemic drugs 4. Insulin Diet The
dietary advice for people with diabetes has changed considerably over
the last few decades. Earlier people with diabetes were asked to starve
themselves! Later people with diabetes were told to avoid all sugars and
starches. Today, however, the principle is to eat healthily, in the same
way that is recommended for the whole population, with few
modifications.
A balanced diet based on starchy foods and lots of fruits and
vegetables, and is low in fat, salt and sugar.
What is important to know is what to eat, when to eat and how much
you should eat.
Effective management of diabetes cannot be achieved without
appropriate dietary modifications.
All newly diagnosed patients with diabetes should receive advice on
life style and dietary modification from their `Diabetic team`.
The aims of these dietary advices are to provide you with knowledge
of healthy eating, encourage lifestyle modifications in order to reduce
obesity and ensure optimal weight, to maintain blood sugar and
cholesterol levels as near normal as possible. Good dietary advice and
following them properly may reduce the risk of acute complications of
diabetes like low blood sugar reaction (hypoglycaemia) and high levels
of blood sugar (hyperglycaemia).
Your diet should provide 50% energy intake from complex
carbohydrates, such as that found in whole grain food stuff, which
absorbs slowly. This prevents rapid rise in blood glucose level. Avoid
rapidly absorbed carbohydrates, like sugar, desserts etc.
You must reduce the consumption of food stuff like butter, cheese,
sausages etc to limit the fat intake to less than 30% energy uptake.
Instead of having three “large” main meals, try to reduce the
quantities of main meals and have sugar/fat free snacks in between. This
helps you to maintain a stable blood sugar level throughout the day.
(Having six small meals is better than having three large meals and no
snacks)
Exercise and diabetes
Exercise plays a major role in the management of diabetes. Physical
activity can help you control your blood glucose, weight, and blood
pressure, as well as raise your “good” cholesterol and lower your “bad”
cholesterol. It can also help prevent heart and blood flow problems,
reducing your risk of heart disease. Exercise helps you relax and can
also help you feel better about yourself and increase your overall
health.
The journey of a thousand miles begins with a single step. Exercise
works the same way. Taking that first step can be hard, especially if
you’ve been diagnosed with diabetes. Remember — it’s never too late. You
can always improve your level of fitness.
For most people, it is best to aim for a total of 30 minutes of
exercise a day, at least 5 days a week. However one can divide one’s
activity for the day into 2 sessions, 15 minutes each.
An often heard excuse is that the patient does not have the time to
engage in exercise. This is not an acceptable excuse. The lack of time
factor can be addressed in some simple, practical ways(, eg. By getting
off the bus 3 or 4 stops before the destined regular stop and walking
part of the way.)
If one has to do marketing on foot, by taking a circuitous route one
could get the requisite exercise without a time constraint.
One could use one’s own ingenuity to get the quota of exercise
without making it look like a burden.
Benefits of exercise
1. Exercise burns calories, which will help you lose weight and
maintain a healthy weight.
2. Exercise can help your body respond to insulin better and may
reduce the amount of insulin needed to maintain good blood glucose
levels.
3. Exercise can improve your circulation, especially in your arms and
legs, where people with diabetes can have problems.
4. Exercise helps reduce stress, which can raise your glucose level.
5. It can lower your risk of heart disease
6. It reduces your cholesterol levels
7. It helps you control your blood pressure.
8. In some people, exercise and a proper diet can control Type 2
Diabetes without the need for medications.
Now that you know the benefits of exercise, you are ready to start
your exercise program.But if you have recently been diagnosed as having
diabetes have been inactive and out of shape not had experience with
diet or insulin adjustment,have had complications from diabetes have
other health problems such as high blood pressure, heart diseases, joint
diseases etc Meet your doctor before you begin an exercise program. Your
doctor can tell you about the kinds of exercise that are good for you
depending on how well your diabetes is controlled, any complications you
may have had or other health related conditions.
What kind of exercise should you do? Most doctors recommend aerobic
exercise, which makes you breathe more deeply and makes your heart work
harder. Examples of aerobic exercise include brisk walking, jogging,
swimming or bicycling. There is another type of exercise and this
improves flexibility, coordination and muscle tone (eg: ankle rotation,
arm circles and stretching muscles). Depending on your health status
your doctor will recommend the type of exercise that suits you the most.
For example if you have problems with the nerves in your feet or legs,
your doctor may want you to do a type of exercise that won’t put stress
on your feet. These exercises include swimming, bicycling, rowing or
chair exercises.
No matter what kind of exercise you do, when you start an exercise
program, go slowly. Gradually increase the intensity and length of your
workouts as you get fitter .Remember you should warm up before you start
and cool down when you are done.
To warm up, spend 5 to 10 minutes doing a low-intensity exercise such
as walking. Then gently stretch for another 5 to 10 minutes. Repeat
these steps after exercising to cool down.
Exercise and low blood sugar reaction (Hypoglycaemia) Your health
care team will discuss with you about the possibility of low blood sugar
reaction (hypoglycaemia) which is a potential risk for a person with
diabetes. This usually occurs while exercising or immediately after
activity. But you should keep in mind the possibility of having a
reaction even few hours afterwards.
You should be alert to the symptoms of hypoglycaemia and should never
ignore the warning signs. When your blood sugar level drops below a
critical level you may feel a change in your heartbeat, sweat
excessively, get a headache, feel dizzy, become anxious and shaky, and
feel irritable.
Or you may get a tummy pain, nausea or feel very hungry. If you
ignore the initial warning symptoms your sugar level will drop
drastically and you may even lose consciousness.
At the first sign of above symptoms, you should stop exercising and
follow your doctor’s advice about how to treat hypoglycaemia. Your
doctor may suggest you keep some toffees, packet of glucose/sugar or
juice at hand to treat hypoglycaemia. It is important to remember, if
you do have an attack of hypoglycaemia and even if you are treated
promptly, it could recur during the course of the day. Be under medical
supervision till the episode is clearly behind you.
Some exercise tips
If you’re planning to walk or jog, be sure you wear comfortable well
fitting shoes. When ever possible wear socks. Be on the look out for
blisters.
Stretch for five minutes before and after your workout regardless of
how intense you plan to exercise. Start slowly with a low-impact
exercise such as walking, swimming, or biking.
Build up the time you spend exercising gradually. If you have to,
start with five minutes and add a bit of time each day.
Drink plenty of fluids while you exercise, especially when it’s hot.
Dehydration can increase your blood sugar. If you exercise for more
than an hour, drink carbohydrate-containing beverages rather than plain
water.Monitor your blood glucose levels before, if possible during (at
least initially), and after exercise to assess your requirements for
extra food.
Discuss adjusting carbohydrate intake with your doctor/dietitian.
Adjust insulin and medication.
In Western countries diabetics always wear a diabetes identification
tag indicating that they have diabetes to ensure proper treatment in
case of an emergency.
Have some chocolate, toffees, fruit juice, sugar tablets or glucose
handy in case of low sugar reaction. If you experience any warning
signs, stop exercising. If you don’t feel better within 15 minutes, seek
immediate medical help.
Oral hypoglycaemic drugs
Controlling your blood sugar is essential to feeling healthy and
avoiding long-term complications of diabetes. Some people are able to
control their blood sugar with diet and exercise alone. When diet,
exercise and maintaining a healthy weight aren’t enough, you may need
the help of medication. There are different classes of oral medications
available.
Oral medications may include: Sulfonylurea drugs (eg Glibenclamide,
Gliclazide, Glipizide), which stimulate the production of insulin in the
pancreas. Most common side effect is low blood sugar reaction (hypoglycaemia)
especially during the initial period of therapy.
Biguanides (eg Metformin), which decrease the amount of sugar made
and released from the liver, hence you need less insulin to transport
blood sugar into the cells. Another added advantage is, this group of
drugs produce less weight gain. Side effects include a metallic taste in
your mouth, loss of appetite, nausea or vomiting, abdominal bloating,
and rarely diarrhoea. It is advisable to take this medication with food
to avoid these side effects .A rare but serious side effect is lactic
acidosis, which results when lactic acid builds up in your body.
Symptoms include tiredness, weakness, muscle aches, dizziness and
drowsiness.
Alpha-glucosidase inhibitors (eg Acarbose), which slow down the
absorption of starches. This helps prevent the rapid rise in blood sugar
that usually occurs right after a meal. Commonly patients complain of
abdominal bloating. Higher doses can cause liver damage as well.
Meglitinides (eg Repaglinide, Neteglinide), which stimulate the
production of insulin in the pancreas just like sulfonylurea drugs. But
hypoglycaemia is not as common.
Thiazolidinediones (eg Pioglitazone, Rosiglitazone), which makes the
body more sensitive to insulin and keep the liver from overproducing
sugar. Side effects include, weight gain and fatigue. There is a
possibility of liver damage and if you are being prescribed this drug
your doctor will advice you to check your liver functions every two
months during the first year of treatment. You must contact your doctor
immediately if you experience any of the signs and symptoms of liver
damage, such as nausea and vomiting, abdominal pain, loss of appetite,
dark urine, or yellowing of your skin and the whites of your eyes
(jaundice). These may not always be related to diabetes medications, but
your doctor will need to investigate all possible causes.
Drug combinations
Sometimes your doctor may decide to combine two or three drugs from
different classes for better blood sugar control. Each class of oral
medication can be combined with drugs from any other class.
Insulin is a hormone that controls the level of blood sugar (also
called glucose) in your body.
When we eat, our body breaks food down into organic compounds, one of
which is glucose.
The cells of our body use glucose as a source of energy for movement,
growth, repair, and other functions. But before the cells can use
glucose, it must move from the bloodstream into the individual cells.
This process requires insulin.
Insulin is produced by some small cells in the pancreas (beta cells).
When glucose enters our blood stream, the pancreas should automatically
produce the right amount of insulin to move glucose into our cells.
If the beta cells degenerate so that the body cannot make enough
insulin on its own, Type I diabetes results. A person with this type of
diabetes must inject exogenous insulin (insulin from sources outside the
body).
In Type II diabetes, the beta cells produce insulin but this amount
is either not enough or the cells throughout the body do not respond
normally to it. Nevertheless, insulin also may be used in type II
diabetes to help overcome the resistance of cells to insulin.
By reducing the concentration of glucose in the blood, insulin is
thought to prevent or reduce the long-term complications of diabetes,
including damage to the blood vessels, eyes, kidneys, and nerves.
Types of Insulin
There are more than 20 types of insulin products available in four
basic forms, each with a different time of onset and duration of action.
The decision as to which insulin to choose is based on an individual’s
lifestyle, a physician’s preference and experience, and the person’s
blood sugar levels. Among the criteria considered in choosing insulin
are: how soon it starts working (onset) when it works the hardest (peak
time) how long it lasts in the body (duration).
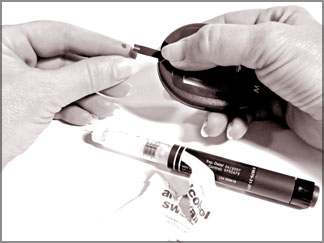
What are the types of Insulin Delivery Devices? All insulin delivery
devices inject insulin through the skin and into the fatty tissue below.
Most people inject insulin with a syringe that delivers insulin just
under the skin. Others use insulin pens, jet injectors, or insulin
pumps.
Several new approaches for taking insulin are under development.
Syringes are hypodermic needles attached to hollow barrels that
people with diabetes use to inject insulin. Insulin syringes are small
with very sharp points. Most have a special coating to help the needles
enter the skin as painlessly as possible. Insulin syringes come in
several different sizes to match insulin strength and dosage.
Insulin pens look like pens with cartridges - but the cartridges are
filled with insulin rather than ink. They can be used instead of needles
for giving insulin injections. Some pens use replaceable cartridges of
insulin; other models are totally disposable after the pre-filled
cartridge is empty. A fine short needle, like the needle on an insulin
syringe, is on the tip of the pen. Users turn a dial to select the
desired dose of insulin and press a plunger on the end to deliver the
insulin just under the skin.
Insulin jet injectors may be an option for people who do not want to
use needles. These devices use high pressure air to send a fine spray of
insulin through the skin. Jet injectors have no needles. In Sri Lanka
jet injectors are hardly used.
Insulin Pumps
Insulin pumps are small pumping devices worn outside of your body.
They connect by flexible tubing to a catheter that is located under the
skin of your abdomen. You program the pump to dispense the necessary
amount of insulin. Usually, you set the pump to give a steady small dose
of insulin, but you can give an additional amount in a short time if
needed, such as after a meal.
If adjusted properly, these pumps allow close control of your insulin
levels without multiple injections. You should not use this type of pump
during physical activities that may damage the pump or disrupt the
pump’s connection to the body. You still need to monitor your blood
glucose levels regularly if you use this type of device. Insulin pumps
are not commonly used in Sri Lanka.
What information should my doctor have before starting insulin?
Before using this preparation make sure your doctor or pharmacist knows:
if you are pregnant, trying for a baby or breast-feeding if you suffer
from kidney problems if you have ever had an allergic reaction to
insulin or any other medicine if you are taking any other medicines,
including those which could be bought without a prescription, herbal or
complementary medicines What are the goals of insulin treatment?
The goal of insulin treatment is to keep blood glucose levels at
normal or near-normal levels. Careful control of blood glucose levels
can help prevent both the short-term effects of poorly controlled blood
glucose and the long-term effects of poorly controlled blood glucose
(diabetic complications of the eye, kidney, nerves and heart).
How to use insulin? Use your medication exactly as directed. Try to
have your injection at the same time each day. Before you inject, if you
have pre-drawn your insulin in the syringe, take it out from the
refrigerator half an hour before injection Your doctor will show you how
to inject yourself with insulin. It is usually injected into the upper
arms, thigh, buttocks or abdomen.Always read the printed information
leaflet, if possible before beginning treatment.Some types of insulin
require mixing, check with your doctor if you are unsure. Mix insulin
well by rolling the bottle slowly between the hands or by tipping the
bottle upside down and gently rotating about 10 times.
Do not shake the insulin as frothing or bubbling can cause an
incorrect dose.
Insulin doses are referred to in terms of units.
Clean the skin before, and after injecting.
Eat 20 - 30 minutes after your injection.
Never take more than the prescribed dose. If you suspect that you or
someone else has taken an overdose of this preparation immediately take
some sugar/glucose because hypoglycaemia can kill you. Then you contact
your doctor or go to your local hospital at once. Always take the
container with you, if possible, even if empty.
This medicine is for you. Never give it to others even if their
condition appears to be the same as yours.
Carefully dispose of your used needles and syringes in a used bottle
with a screw cap.
Where should I inject the Insulin? The usual places to inject insulin
are the upper arm, the front and side of the thighs, and the abdomen
(tummy area). Ask your doctor which place you should use. Insulin
injected near the stomach works fastest, while insulin injected into the
thigh works slowest. Insulin injected into the arm works at medium
speed. Some prefer the abdomen as it is easy to inject than limbs and
the rate of absorption is fairly constant.
It is important to rotate your injection sites because repeated
injection at the same site causes fat to accumulate at that area. This
results in poor absorption of the insulin when injected. It is also
unsightly.
Shift each injection site by 1 finger space and do not inject bruised
area.
If you take too much insulin it will lower your blood sugar level too
much, and you may get hypoglycaemia (also called an insulin reaction).
When you have hypoglycaemia, you may feel sweaty, more tired than usual,
confused and shaky, and you may feel drowsy. In serious cases, you can
pass out or have a seizure (a fit). Talk to your doctor about how to
treat hypoglycaemia. Your doctor may suggest that you always carry a
snack with you, such as candy, fruit juice or glucose, to treat
hypoglycaemia.
Storage of Insulin Write the date on the bottle when you open it.
An opened bottle of insulin will expire 2 months after it is opened
and must be discarded at this time Keep the opened bottle of insulin
with syringes to be used again in a box Never freeze insulin; keep it in
the middle compartment of refrigerator.
Penfill cartridges do not require refrigeration when they are in use.
Do not leave insulin in the sun or unattended in your car.
Getting the most from your treatment. As no two people are alike,
treatment may consist of one or more types of insulin with the amounts
you use carefully chosen to suit your requirements.Before taking any
‘over-the-counter’ medicines, check with your pharmacist which medicines
are safe for you to take alongside this preparation.
Keep your regular appointments with your doctor. You must test for
sugar in the blood or urine to make sure that you are taking the right
dose of insulin for you. Your doctor will show you how to test your
blood sugar and how to use the results of the test.
Do not drink alcohol on an empty stomach as this could cause severe
hypoglycaemia (low blood sugar).
Check with your doctor before taking up any physical exercise as this
will have an effect on your blood sugar levels, which can last for
hours.
Check with your doctor if you develop an infection, you may need a
change in dosage.
Check you have been given the correct insulin each time you collect
your prescription.Change the injection site on your body regularly to
help prevent skin problems and difficulties in injecting.
Keep at hand an extra supply of insulin and an injection device, a
blood or urine testing strip and a source of sugar.
The writer is attached to the Colombo South Teaching
Hospital,Kalubowila. |
