|

Dr Gopi Kitnasamy |
Overdose of chromosome 21
Down syndrome is the commonest chromosome abnormality
in humans, but early interventions can improve physical and mental
disabilities:
By Carol Aloysius
World Down Syndrome (DS) Day was
observed recently. Apart from the delay in cognitive ability (mental
retardation) and physical growth that usually occur as a result of DS,
which begins in early childhood, the disease also adversely affects the
bones and joints, hampering the movements of the child. These negative
impacts however can be largely reduced with early interventions.
Chartered Physiotherapist, Dr Gopi
Kitnasamy, explains how the disease is caused and why early
physiotherapy should be initiated.
Excerpts…
Q:What exactly is Down syndrome?
A: Down Syndrome (DS) or Down’s syndrome, also known as
trisomy 21, is a chromosomal condition caused by the presence of all or
part of a third copy of chromosome 21. Down syndrome is the most common
chromosome abnormality in humans. This extra chromosome changes the
normal development of the body and brain. It is typically associated
with a delay in cognitive ability (mental retardation, or MR) and
physical growth, and a particular set of facial characteristics. Almost
all of the conditions that affect the bones and joints of people with
Down syndrome arise from the abnormal collagen found in Down syndrome.
Collagen is the major protein that makes up ligaments, tendons,
cartilage, bone and the support structure of the skin. One of the types
of collagen (type VI) is encoded by a gene found on the 21chromosome.
The resulting effect in people with DS is increased laxity, or
looseness, of the ligaments that attach bone to bone and muscle to bone.
 The
combination of this ligamentous laxity and low muscle tone contribute to
orthopedic problems in people with Down syndrome. Motor function in
individuals with Down syndrome is characterised by hypotonia and
hyperflexibility, which results in an increased risk of joint
dislocation and retarded motor skills. Hypotonia, decreased muscle tone,
has a negative effect on the proprioceptive feedback from muscle and
joint sensory structures and can have a detrimental effect on the
efficiency of co-contractions and postural reactions. People with Down
syndrome have more joint mobility than the average. The enlarged joint
mobility may contribute to the lack of posture control. Together with
the failure of co – contraction, it will affect the joint stability. The
combination of this ligamentous laxity and low muscle tone contribute to
orthopedic problems in people with Down syndrome. Motor function in
individuals with Down syndrome is characterised by hypotonia and
hyperflexibility, which results in an increased risk of joint
dislocation and retarded motor skills. Hypotonia, decreased muscle tone,
has a negative effect on the proprioceptive feedback from muscle and
joint sensory structures and can have a detrimental effect on the
efficiency of co-contractions and postural reactions. People with Down
syndrome have more joint mobility than the average. The enlarged joint
mobility may contribute to the lack of posture control. Together with
the failure of co – contraction, it will affect the joint stability.
Q: You referred to several musculoskeletal problems that
persons with DS are likely to suffer from. What are the most common and
which part of the body is most affected?
A: The most common musculoskeletal problems in Down syndrome are:
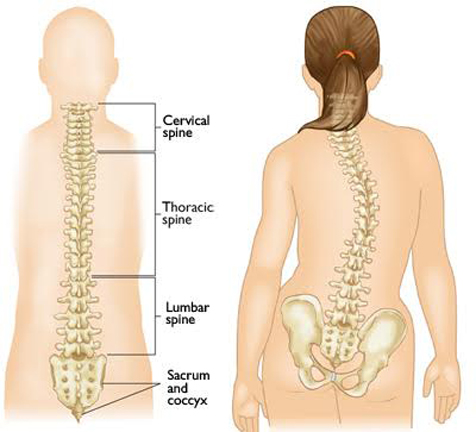
*Spine - Atlantoaxial instability, which is the looseness between the
first and second vertebrae of the neck.
* Scoliosis, which is the curvature of the spine to the side.
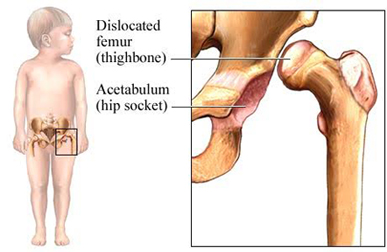
* Hip - five to eight percent of children with DS will develop
abnormalities of the hip. With regard to the hip, the most common
condition is dislocation of the hip, which is also called subluxation.
In this condition, the head of the thigh bone (the femur) moves out of
the socket formed by the pelvis (the acetabulum). This dislocation may
or may not be associated with malformation of the acetabulum. The
dislocation appears to be due to a combination of laxity of the
connective tissue that normally keeps the hip together along with the
low muscle tone found in DS.
|
What Causes Down
Syndrome?
The cause of the extra full or partial
chromosome is still unknown. Maternal age is the only factor
that has been linked to an increased chance of having a baby
with Down syndrome resulting from nondisjunction or
mosaicism. However, due to higher birth rates in younger
women, 80% of children with Down syndrome are born to women
under 35 years of age.
There is no definitive scientific research
that indicates that Down syndrome is caused by environmental
factors or the parents’ activities before or during
pregnancy. The additional partial or full copy of the 21st
chromosome which causes Down syndrome can originate from
either the father or the mother. Approximately 5% of the
cases have been traced to the father.
What is the likelihood
of having a child with Down syndrome?
Down syndrome occurs in people of all
races and economic levels, though older women have an
increased chance of having a child with Down syndrome. A 35
year old woman has about a one in 350 chance of conceiving a
child with Down syndrome, and this chance increases
gradually to 1 in 100 by age 40. At age 45 the incidence
becomes approximately 1 in 30. The age of the mother does
not seem to be linked to the risk of translocation.
Does down syndrome run in families?
All 3 types of Down syndrome are genetic
conditions but only 1% of all cases of Down syndrome have
a hereditary component. Heredity is not a factor in trisomy
21 (nondisjunction) and mosaicism. However, in one third of
cases of Down syndrome resulting from translocation there is
a hereditary component - accounting for about 1% of all
cases of Down syndrome.
How is Down syndrome diagnosed?
Prenatally
There are two categories of tests for Down
syndrome that can be performed before a baby is born:
screening tests and diagnostic tests. Prenatal screens
estimate the chance of the fetus having Down syndrome. These
tests do not tell you for sure whether your fetus has Down
syndrome; they only provide a probability. Diagnostic tests,
on the other hand, can provide a definitive diagnosis with
almost 100% accuracy.
At
Birth
Down syndrome is usually identified at
birth by the presence of certain physical traits: low muscle
tone, a single deep crease across the palm of the hand, a
slightly flattened facial profile and an upward slant to the
eyes. Because these features may be present in babies
without Down syndrome, a chromosomal analysis called a
karyotype is done to confirm the diagnosis. Another genetic
test called FISH can apply similar principles and confirm a
diagnosis in a shorter amount of time. |
Q: Is this abnormality detected at birth?
A: Interestingly, hip subluxation in children with Down
syndrome is hardly ever found at birth but instead is most common
between the ages of 3 and 13 years. The most common sign is a limp, and
pain may or may not be present.
Other parts of the body that are affected include:
 *
Knee - Instability of the patella (kneecap) has been estimated to occur
in close to 20 per cent of people with DS. The majority of cases of
instability present only as kneecaps that can be moved further to the
outside than the normal kneecap (subluxation); however, some people can
have their kneecaps completely move out of position (dislocation), and
some may even have a hard time getting it back into the right position.
Mild subluxation of the kneecap is not associated with pain, but
dislocation may be painful. While people with instability of the patella
are able to walk, there is often a decreased range of motion of the
knee, with an accompanying change in gait. The longer nothing is done
for the instability, the worse the condition will get over time. *
Knee - Instability of the patella (kneecap) has been estimated to occur
in close to 20 per cent of people with DS. The majority of cases of
instability present only as kneecaps that can be moved further to the
outside than the normal kneecap (subluxation); however, some people can
have their kneecaps completely move out of position (dislocation), and
some may even have a hard time getting it back into the right position.
Mild subluxation of the kneecap is not associated with pain, but
dislocation may be painful. While people with instability of the patella
are able to walk, there is often a decreased range of motion of the
knee, with an accompanying change in gait. The longer nothing is done
for the instability, the worse the condition will get over time.
|
Detected at birth
A consultant neurologist speaking in a
telephone interview on grounds of anonymity said Down
Syndrome is usually detected at birth, going on the physical
appearance of the child, with older mothers being more at
risk of giving birth to such children. Once a child has been
diagnosed with DS, parents should not adopt a negative
attitude. “Rather, they should seek early advice on how they
can help them to develop. If exposed to stimulation at a
younger age, the better the outcome for the child. The
important thing is for parents to seek professional advice
like occupational therapy and interact with their children
at all stages of their development, however slow. They must
continue to do this and watch their improvements however
small,” the neurologist emphasised. |
*Foot - Flat foot, also called ‘pes planus’, is seen in the vast
majority of people with DS. In mild cases, the heel is in a neutral
position. In severe cases, the heel rotates so that the person is
walking on the inside of the heel.
* Metatarsus primus varus is also commonly seen in people with DS.
This is a condition in which the front part of the foot behind the big
toe bends inward.
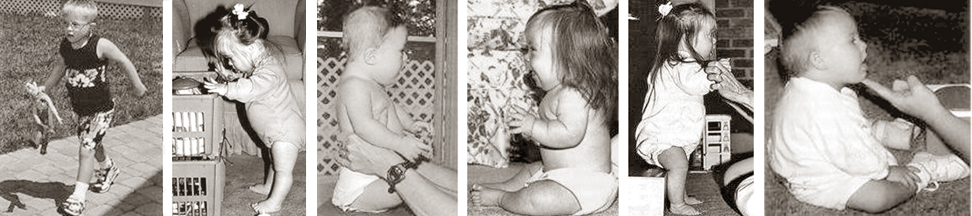
Q: So how does physiotherapy help these children?
A: The goal of physiotherapy for children with DS is not to
accelerate their rate of gross motor development as is commonly assumed.
The goal is to improve the near normal gross motor development and
minimise the development of abnormal compensatory movement and posture
patterns that children with DS are prone to develop. Early physiotherapy
makes a decisive difference in the long-term functional outcome of the
child with DS. The gross motor development is the first learning task
that the child with DS encounters; it provides parents with the first
opportunity to explore how their child learns. There is increasing
evidence that the children with DS have a unique learning style.
Q: Do parents and carers have a role in this exercise?
A: Understanding how children with DS learn is crucial for
parents who wish to facilitate the development of gross motor skills as
well as facilitating success in other areas of life including language,
education and the development of social skills.
Normal gait or walking is very important. Ligamentous laxity,
hypotonia and weakness in the legs lead to lower extremity posturing
with hip abduction and external rotation, hyperextension of the knees
and pronation and eversion of the feet. Children with DS typically learn
to walk with their feet wide apart, their knees stiff and their feet
turned out.
 They
do so because hypotonia, ligamentous laxity and weakness make their legs
less stable. Locking their knees, widening their base and rotating their
feet outward are all strategies to increase stability. The problem
however is that this is an inefficient gait pattern for walking. The
weight is being borne on the medial (inside) borders of the feet, and
the feet are designed to have the weight borne on the outside borders.
If this pattern is allowed to continue, problems will develop with both
the knees and the feet. Walking will become painful, and endurance will
be decreased. Physiotherapy should begin teaching the child with DS the
proper standing posture (i.e., feet positioned under the hips and
pointing straight ahead with a slight bend in the knees) when he or she
is still very young. With appropriate Physiotherapy, gait problems can
be minimised or avoided. They
do so because hypotonia, ligamentous laxity and weakness make their legs
less stable. Locking their knees, widening their base and rotating their
feet outward are all strategies to increase stability. The problem
however is that this is an inefficient gait pattern for walking. The
weight is being borne on the medial (inside) borders of the feet, and
the feet are designed to have the weight borne on the outside borders.
If this pattern is allowed to continue, problems will develop with both
the knees and the feet. Walking will become painful, and endurance will
be decreased. Physiotherapy should begin teaching the child with DS the
proper standing posture (i.e., feet positioned under the hips and
pointing straight ahead with a slight bend in the knees) when he or she
is still very young. With appropriate Physiotherapy, gait problems can
be minimised or avoided.
Trunk position or spinal posture is another important consideration
for physiotherapy. Ligamentous laxity, hypotonia and decreased strength
in the trunk encourage the development of kyphosis or Scoliosis, which
is often first seen when the child is learning to sit. Children with DS
typically learn to sit with a posterior pelvic tilt, trunk rounded and
the head resting back on the shoulders. They never learn to actively
move their pelvis into a vertical (upright) position, and therefore,
cannot hold their head and trunk over it. If this posture is allowed to
persist, it will ultimately result in impaired breathing and a decreased
ability to rotate the trunk.
The other important goal is to facilitate the development of optimal
motor movement patterns. Children often develop adaptations that help
them achieve movement but can lead to musculoskeletal injuries over the
long term. Physiotherapy helps prevent these non-ideal patterns from
developing and prevent developing other musculoskeletal problems.
 |

