|
observer |
|
|
|
|
|
OTHER LINKS |

|

|

|
Provide a supportive workplace environment for victims of AIDS:Let them also live"Stone them! Stone them", was the cry they were hearing from around the neighbourhood. The family of four, parents and the two young daughters were trapped. Fear, gripped Padma (not her real name).
What caused the change? Just the previous day Padma's husband had been diagnosed as HIV+ at the Colombo National Hospital. Though the family had hidden the truth, a minor staff member of the hospital, from the same village had done the deed. "My husband fled for life. The poor darling! He had roamed the streets for days and had taken poison, attempting to commit suicide." Fortunately, her husband's life was saved at another hospital. Is HIV/AIDS different from other illnesses, for the society to drive people who are living with HIV/AIDS to seclusion, hiding or suicide? What is HIV/AIDS? The Human Immune-deficiency Virus (HIV) is a virus that decreases the ability of the human body to fight disease. Acquired Immune Deficiency Syndrome (AIDS) is its developed stage. With specific and limited ways of infection. It spreads through blood with a 100 per cent possibility. Other ways of infection are through unprotected sexual intercourse and from mother to child, during natural childbirth and through breast milk. A virus with very limited modes of infection, what brings in so much attention to this disease? Human behaviour is the key. Spread mainly through unprotected sex, HIV/AIDS had affected millions of lives through the globe. (25 M deaths, and 40 M living with HIV/AIDS by end 2005 - UNAIDS). In 2001, United Nations declared it a 'global emergency'. UN member countries gathering at New York, USA, at a Special Session of the General Assembly vowed to combat the virus. The declaration agreed therein, was signed by 189 member countries including Sri Lanka, committing the country to achieve 17 concrete, time-bound international targets. TargetsThe first set of targets, assessed in 2003, focused on establishing frameworks for a national policy to enable and stimulate effective action against the spread of HIV/AIDS. Development and implementation of multisectoral national strategies and financing plans; integration of care, treatment, support and impact mitigation priorities into the mainstream of development planning; establishing time bound national target to recuce prevalence among young men and women aged 15 to 24 years; implementing universal precautions in health-care settings; establishing effective monitoring systems; and enacting legislation, regulation and other measures to eliminate all forms of discrimination and to ensure enjoyment of human rights and fundamental freedoms by people living with HIV/AIDS and vulnerable groups, were some of the targets that Sri Lanka needed to meet by end of 2003.
A review session of the UN General Assembly - UNGASS + 5, commences on May 31, 2006 how has the country performed on achieving UNGASS commitment targets? Sri Lanka's national report on the performance of UNGASS commitments during the period 2003 to 2005, will be presented at the review. The report posted in the public domain of UNAIDS, recording the progress during the period using national commitment indicators, stresses on the 'low prevalent' status of the country. (see Box 1 - National Report, in a nutshell) However, "the lack of policy in many areas: overburdening of technical staff at the NSACP, lack of commitment by administrators in sectors: delays in disbursement and utilisation of funds; delay in awarding large contracts (behavioural surveillance, monitoring, large NGO contracts for targeted interventions), lack of uniformity in implementation of prevention and control activities in health sector subsequent to decentralisation; problems in monitoring and supervision of the peripheral clinics/NGOs and other sectors," are pointed as constraints to the national response on HIV/AIDS. Though the national report takes a positive note, the response lacks strength in many areas, points out a shadow report on 'UNGASS Monitoring Civil Society Perspectives, Sri Lanka' posted on the website of UNGASS-HIV Organisation (www.ungasshiv.org). An endeavour of the Panos Global AIDS Programme (GAP) to identify achievements and challenges on UNGASS commitments, the report points out many loopholes in the national response, at different levels. The report concludes that "Sri Lanka has yet to follow up on many of the commitments made at UNGASS" and lists out six targets yet to be met. * By 2003 implement universal precautions (UP) * By 2003 ensure that national strategies are developed to provide psychosocial care to individual, families and com munities affected by HIV/AIDS * By 2003 enact legislation, regulations and other measures to eliminate all forms of discrimination against PLWHA (persons living with HIV/AIDS) and members of vulnerable groups. * By 2005 ensure access to HIV/AIDS prevention programs to migrant and mobile workers * By 2005 ensure that at least 90% and by 2010 at least 95% of young men and women ages 15-24 have access to information and education on HIV/AIDS * By 2005 implement national strategies to promote and advance women and women's full enjoyment of human rights and reduction of their vulnerability to HIV/AIDS. Reports and technicalities aside, what is the reaction of the common man? The Sunday Observer spoke to persons living with HIV/AIDS and health care personnel. Training of health-care personnel; the practice of universal precautions; right to voluntary and confidential testing and pre and post counselling; right to employment; knowledge of HIV/AIDS and stigma and discrimination were some of the areas checked in relation to UNGASS commitments. KnowledgeHow much knowledge did they have of the virus or its modes of transmission? Almost none, until they had to face the disease themselves. Lalith (not his real name), a 41 year old father of three children, explains that his HIV+ status surfaced only after 12 years of marriage. Though his previous partner being diagnosed with AIDS had died some time before his marriage, he had not tested himself. Padma was better prepared due to her husband's sickness. However, "I have seen posters on HIV/AIDS at dispensaries and clinics but never took an interest because I never dreamt of getting it myself. I was not even aware of the use of condoms", she says. Testing on HIV/AIDS was done as a last resort, after prolonged hospitalization says Lalith. Though there were no pre-counselling sessions, the doctor who attends to him now (private practitioner) counselled him after being tested positive and gave him hope of a healthy life, says Lalith. For Padma, who was tested positive, three months after her husbands death, pre and post counselling had helped to get early medication, and to lead a healthy life. Stigma and discrimination had traumatized Padma and her two young daughters, since the day she had had knowledge of her husbands HIV+ status. However, though it was hard to reveal his status to immediate family, both his parents and in-laws are supportive, says Lalith. However, "none are brave to identify oneself as a positive person due to the stigma and discrimination by the society" they say. Padma, who had been employed at a pre-school, had lost her job after the owner had got to know her HIV status. However, both of them are gainfully employed again and resumed their normal lives. Both Padma and Lalith pointed out the 'damaging effect' of insensitive posters and advertisements on AIDS prevention and control. "You are scared to even look at them because they talk of death rather than AIDS. HIV/AIDS is portrayed as death. This brings in fear and increases stigmatization and discrimination of PLWHA. The more the society discriminates PLWHA, the more they tend to hide. Unless they come out and disclose their illness they could not be treated and counselled, preventing spread of the illness. How do we know who is already infected, nobody discloses," they explained. A Sister and Ward Incharge Nurse of an STD/AIDS clinic close to Colombo, who preferred not to be identified pointed out that in their clinic, there was no discrimination. Universal precautionary proceduresUniversal precautionary procedures were adhered to and confidentiality is valued "because otherwise the patient will not come back for treatment, which is vital to keep the virus in check". However, they said there is a dearth of trained health-care workers on HIV/AIDS. "Even the two of us only have the in-service training, or training received by working with patients at the clinic", they stated. Dr. Ananda Wijewickrema, in charge of a special HIV/AIDS ward within the periphery of Colombo, agreed that health-care workers needed more training. "I had the experience of training for two weeks in Thailand, not only the doctors, but most importantly those who interact more with the patient and families, the nurses and minor staff should get this kind of training" he said. Non-availability of medication at the STD clinics hampers the process, he said. "The patient could be from Anuradhapura, but still he or she will have to come to Colombo STD clinic for his or her free medication. There should be some plan to provide them treatment and medication at an accessible location" he said. ***** Sri Lanka is a role modelInterview with Dr. Kulasiri Buddhakorala: Question: In NSACP perspective, what were the expectations from Sri Lanka in accordance with the UNGASS declaration on HIV/AIDS? A: Sri Lanka being a low prevelance country inspite of high mobility of the population and other high risk behaviours UNGASS expects through a concerted effort Sri Lanka would continue as a low prevelance country in the years to come. Q: How far has Sri Lanka been able to meet these targets? A: Keeping with WHO '3 by 5' initiative NSACP was able to provide ARV treatments for eligilble HIV/AIDS patients. Q: If targets/goals were not met, what are the reasons (NSACP view) and who is/are responsible? A: Certain service provisions have not been expanded in the entire country e.g. VCT services. Testing facilities should be expanded in needy places with the collaboration of other healthcare facilities. Trained healthcare personnel should be available in the provinces. Q: When it comes to the issue of HIV/AIDS, what advantages or disadvantages does Sri Lanka have? A: Sri Lanka is unique and a role model to other countries in the region and the world, being a low prevalence country with factors for an explosive epidemic. High literacy rate and readiness to listen to a health message, readiness to change behaviour are contributory factors for low prevelance. Q: What are the three main problems arising from HIV/AIDS that Sri Lanka is faced with? A: No major problems have been encountered because of the low number of patients. Stigma and discrimination still exists to a lesser degree. High index of clinical suspicion from clinicians when dealing with patients in healthcare settings. Q: What awaits in the future (plans, hopes and fears about the country programme)? A: Plans are ready for the next three years to respond to HIV/AIDS. Hopes are high on the horizon that Sri Lanka would not face an explosive epidemic. |
 Would they live through the night? Tears stream down Padma's face as
she re-lives that fateful night, as she tells how, neighbours, friends
of the family turned against them within one night.
Would they live through the night? Tears stream down Padma's face as
she re-lives that fateful night, as she tells how, neighbours, friends
of the family turned against them within one night. 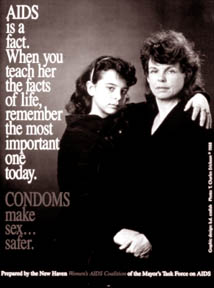 The next set of targets, to be met by 2005 and 2010, focusing on
prevention, care and impact alleviation programmes include providing a
supportive workplace environment for people living with HIV/AIDS;
providing information, education and communication in languages most
understood, access to voluntary and confidential counselling and
testing, access to essential commodities including condoms and sterile
injecting equipment, developing and accelerating the implementation of
national strategies promoting advancement of women and full enjoyment of
human rights; promoting shared responsibility of men and women to ensure
safe sex; and implementing measures to increase capacities of women and
adolescent girls to protect themselves from HIV infection.
The next set of targets, to be met by 2005 and 2010, focusing on
prevention, care and impact alleviation programmes include providing a
supportive workplace environment for people living with HIV/AIDS;
providing information, education and communication in languages most
understood, access to voluntary and confidential counselling and
testing, access to essential commodities including condoms and sterile
injecting equipment, developing and accelerating the implementation of
national strategies promoting advancement of women and full enjoyment of
human rights; promoting shared responsibility of men and women to ensure
safe sex; and implementing measures to increase capacities of women and
adolescent girls to protect themselves from HIV infection.