
Early diagnosis, surgical treatment essential
Ectopic pregnancy:
Dr. Vijith Vidyabhushana - Consultant Obstetrician &
Gynaecologist, Colombo South Teaching Hospital, Kalubowila
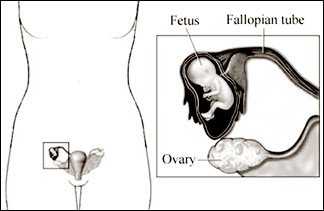
What is an Ectopic pregnancy? An ectopic pregnancy is a pregnancy
occurring in a place, outside the cavity or lining of the womb. The word
‘ectopic’ is derived from the Greek word ‘ektopos’ which means ‘out of
place’. In a normal pregnancy, the fertilised egg implants in the lining
of the womb (Endometrium).
 Over
95% of these ectopic pregnancies occur in the tubes connecting the
ovaries to the womb (These tubes are called fallopian tubes). They can
also happen in one of the ovaries, in the abdominal cavity, or in the
neck of the womb (cervix). Over
95% of these ectopic pregnancies occur in the tubes connecting the
ovaries to the womb (These tubes are called fallopian tubes). They can
also happen in one of the ovaries, in the abdominal cavity, or in the
neck of the womb (cervix).
How common is it? Approximately, out of 100 women who get pregnant 1
is an ectopic pregnancy. In fact, researchers believe ectopic
pregnancies probably happen much more frequently than this. But, many go
unnoticed and unrecorded because a lot of ectopic pregnancies end in
early miscarriage, often before missing a period and therefore before a
woman realises she is pregnant.
How do ectopic pregnancies occur? To understand this it is essential
to understand how the fallopian tubes work under normal conditions.
The fallopian tubes (Tubes connecting the womb to ovaries) are small,
hollow muscular tubes each about ten centimetres long. The outer half is
wider in diameter and lies next to its ovary.
There is a delicate lining inside the tube which is thrown up into
folds which almost fill each tube.
The diameter and the number of folds increases as the tube nears the
ovary and there are tiny finger-like projections at the end of the tube
called fimbria. The purpose of fimbria is to catch the ovum(Egg) and
direct it into the fallopian tubes at the time of ovulation(release of
an egg from the ovary is called ‘ovulation’).
In the lining of these tubes, half the cells produce a thick watery
substance(mucus) and the other half has tiny hair like projections (celia)
which beat gently to propel these secretions towards the cavity of womb.
Following intercourse, sperms swim up through the neck of the womb to
the cavity of the womb and then to the fallopian tubes, some arriving
within fifteen minutes of being deposited in the vagina.
Fertilization(meeting of male-sperm and female-ovum) occurs in the outer
part of the tube near to the ovary.
Fimbria
If the egg is fertilised in the tube, the combined egg and sperm form
a single cell and then divide. The first cell division into two new
cells takes place after twelve to twenty hours, and successive divisions
occur doubling the number of cells each time.
A bundle of cells(called morula) reaches the womb to burrow into the
lining of the womb, four to seven days after release of the egg from the
ovary. Passage of this is dependent on the action of the lining of the
fallopian tube.
 By
this time, female hormones have prepared the lining cells of the womb (endometrium)
for this purpose. Once it burrows into the lining it starts to form the
future placenta which secretes pregnancy hormones (human Chorionic
Gonadotrophin-hCG) in to mother’s blood. By
this time, female hormones have prepared the lining cells of the womb (endometrium)
for this purpose. Once it burrows into the lining it starts to form the
future placenta which secretes pregnancy hormones (human Chorionic
Gonadotrophin-hCG) in to mother’s blood.
Sometimes this delicately folded tube linings can become damaged by
inflammation or infection, and the transport of a fertilized egg to the
womb may fail.
But this bundle of cells is still trying to develop and has a natural
nature to invade into tissues, so it can burrow in to the lining of the
fallopian tube to form a placenta and a resulting dangerous, life
threatening ectopic pregnancy. If 100 women get pregnant, one would have
an ectopic pregnancy.
What are the effects of an ectopic pregnancy? Ectopic pregnancy is a
potentially life threatening condition, as it can cause severe internal
bleeding following rupture of the tube, since the tube is not
distensible to allow the growing pregnancy to expand. Therefore early
diagnosis and surgical treatment are essential for majority of patients.
Am I at risk of getting an ectopic pregnancy? Some women are at high
risk of getting an ectopic pregnancy.
Women with damaged tubes are particularly at high risk:
After a previous ectopic pregnancy. If there is a previous ectopic
pregnancy the risk increases 10 times. Out of 100 women who have had
ectopic pregnancies in the past, 11 would get another ectopic pregnancy.
After pelvic infection - Mainly chlamydia infection or a history of
fever and pain in lower abdomen which are features of pelvic infection.
Chlamydia is a very common sexually transmitted infection which may give
no symptoms and common tests cannot detect this condition.
After infection or scarring of tubes. Scarring may result from
surgery or Endometriosis.
After surgery of Fallopian tubes (including sterilisation); Due to
congenital abnormalities of the tube.
Even if there is no history of damage to tubes following women are at
high risk.
Women using Intrauterine contraceptive devices(IUD). This is a rare
condition as there is a very low risk of failure of the IUD resulting a
pregnancy.
Women over the age of 35.
Subfertile women who are treated with medication to stimulate ovaries
to produce more eggs.
Women who are having IVF treatment and assisted reproductive
techniques like IUI.
Signs and symptoms
Classical Features of an ectopic pregnancy are abdominal pain,
vaginal bleeding and missed or delayed period with a positive pregnancy
test.
There may be shoulder tip pain, dizziness or spells of fainting. If
there is bleeding in to cavity of the tummy due to the rupture of the
ectopic pregnancy, blood will seep through in to the space between liver
and the diaphragm (Diaphragm is the muscle which separates the chest
cavity from the cavity of the tummy) and irritate the diaphragm.
Since the area of the right shoulder tip and the under surface of the
diaphragm are supplied by the same nerve, the brain thinks that the pain
is arising from right tip of shoulder. Therefore the patient complains
of right shoulder tip pain.
This classical symptoms are not always present and therefore a high
index of suspicion about an ectopic pregnancy should be considered in
any woman of reproductive age who complains of abdominal pain with a
positive pregnancy test.
Symptoms of tummy upset may also be prominent in ectopic pregnancy,
notably diarrhoea and painful defaecation.
You may be feeling light headed or faint, and often this is
accompanied by a feeling of something being very wrong. Other signs such
as paleness, increasing pulse rate, sickness, diarrhoea and falling
blood pressure may also be present.The diagnosis should be strongly
suspected in women with above symptoms with especially with the presence
of risk factors.
To be continued.
Autism
Not more, just different:
FASHION is a strange thing, and many fields are susceptible to it not
least, medicine. There has, for example, been a vogue (among
commentators, if not among doctors) to ascribe the rising number of
cases of autism diagnosed over the past couple of decades to childhood
vaccinations against measles, mumps and rubella.
That this is fashion rather than reality is suggested by the fact
that the explanation proffered in Britain has been that such vaccines
provoke an immune response that damages the nervous system, whereas
Americans have blamed residual mercury in the same vaccines.
It is now pretty well established that vaccination does not create
autism. But the rise in the number of recorded cases is real enough. In
Britain, for example, the rate of diagnosis has risen from 50 per
100,000 in 1990 to 400 per 100,000 today. That must have a cause. And
one popular hypothesis is that this cause, too, is fashion?but among
doctors rather than columnists.
Demonstrating that has been difficult. But a paper in this month’s
Developmental Medicine & Child Neurology, by Dorothy Bishop and her
colleagues at Oxford University, goes a long way towards doing so.
Dr. Bishop reasoned it was unlikely that people now labelled autistic
would, in the past, have been thought healthy, but that it was quite
plausible they might have been given some other diagnosis. With this in
mind, she looked at a group who had been diagnosed as children with a
particular condition that was not autism, and rediagnosed them using
present-day criteria.
Her volunteers were 38 adults or teenagers who had, as children, been
diagnosed as having what is known as developmental language disorder,
rather than autism. (The distinction being that although autism involves
difficulties in communication it also has other symptoms, such as an
inability to empathise with others.) The rediagnosis had two steps.
The researchers interviewed the volunteers, of course. But they also
interviewed their parents. They asked both parents and offspring
questions based on modern tests for diagnosing autism.
The result was that almost a third of her volunteers looked, from the
modern point of view, misclassified. Eight fully met the modern criteria
for autism. A further four fell into what is known as the autistic
spectrum, evincing signs of autism short of the full-blown syndrome.
What were particularly telling were the interviews with parents.
Earlier, similar work had explained the observations away as a change in
symptoms with age, but the parents of Dr. Bishop’s volunteers told
stories of what are now regarded as autistic symptoms appearing in their
children in their early years. Although there is a risk of hindsight
colouring such stories, many of them were so vivid that Dr. Bishop is
convinced they are accurate.
The upshot, subject to larger studies confirming her observations, is
that Dr. Bishop seems to have confirmed the cause of the recent rise of
autism as being a change in the diagnostic criteria.
As a good researcher should be, she is cautious and points out that
finding one cause is not proof that others are not operating. But it now
looks unlikely that there are more autistic people around than there
used to be. It is just that it is now fashionable to acknowledge their
existence.
- Economist
Dull jobs really do numb the mind
Boring jobs turn our mind to autopilot, say scientists - and it means
we can seriously mess up some simple tasks.
Monotonous duties switch our brain to “rest mode”, whether we like it
or not, the researchers report in Proceedings of National Academy of
Sciences.
They found mistakes can be predicted up to 30 seconds before we make
them, by patterns in our brain activity. The team hopes to design an
early-warning brain monitor for pilots and others in “critical
situations”. The scientists say the device would be particularly
suitable for monotonous jobs where focus is hard to maintain - such as
passport and immigration control.
“We might be able to build a device (that could be placed) on the
heads of people that makes these easy decisions,” said Dr. Eichele, of
the University of Bergen, Norway.
“We can measure the signal and give feedback to the user that your
brain is in the state where your decisions are not going to be the right
one.”
In the study, Dr. Eichele and his colleagues asked participants to
repeatedly perform a “flanker task” - an experiment in which individuals
must quickly respond to visual clues.
As they did so, brain scans were performed using functional magnetic
resonance imaging (fMRI).
They found the participants’ mistakes were “foreshadowed” by a
particular pattern of brain activity.
“To our surprise, up to 30 seconds before the mistake we could detect
a distinct shift in activity,” said Dr. Stefan Debener, of Southampton
University, UK.
“The brain begins to economise, by investing less effort to complete
the same task.
“We see a reduction in activity in the prefrontal cortex. At the same
time, we see an increase in activity in an area which is more active in
states of rest, known as the Default Mode Network (DMN).”
This is not a sign of the brain going to sleep, says Debener.
“Autopilot would be a better metaphor,” he explains. “We can assume that
the tendency to economise task performance leads to an inappropriate
reduction of effort, thus causing errors.”
Since this state begins about 30 seconds prior to a mistake being
made, it could be possible to design an early-warning system that alerts
people to be more focused or more careful, said the researchers.
That could significantly improve workplace safety and also improve
performance in key tasks, such as driving, analysis of X-rays, or
airport security screening.
But MRI scanners are neither portable enough nor fast enough to be
practical for these real life scenarios, so the next step is to see if
more mobile EEG devices are able to detect the phenomenon.
A prototype of a wireless, mobile, and lightweight EEG amplifier is
currently in development and could be ready for the market in “10 to 15
years”, says Dr. Debener, who is based at the MRC Institute of Hearing
Research, at Royal South Hants Hospital.
“But first, we must establish what is causing these mistakes,” he
adds.
“We do not know whether the change in brain activity we see has a
causal link to the mistakes. After we establish that, we can try to
develop monitoring devices.”
Story from BBC NEWS
|
