|
Today is National Stroke Day:
Preventing a brain attack
With over 200,000 Lankans struck
down by debilitating paralysis every year, stroke is the 2nd leading
cause of hospital deaths in Sri Lanka, but paying attention to your body
can help avert both death and debilitation, says Dr Harsha Gunasekara
by Carol Aloysius
|
Pic - brianakerr.weebly.com |
Strokes have claimed more lives than HIV, Tuberculosis and Malaria
combined. It has disabled more adults than any other cause in the world
- in Colombo alone, 1 in every 100 has been a victim. In a developing
country like Sri Lanka, the 80% of strokes that hit individuals below
the age of 70 continues to contribute to loss of workforce and inhibit
economic progress. The tragedy however, is that simple awareness and
change that could prevent this leading trigger of Sri Lankan deaths - is
all too often regrettably ignored.
Here, Consultant Neurologist, Sri Jayewardenepura Hospital, Dr Harsha
Gunasekara explains why it is important to pay attention to the smallest
signs and symptoms that indicate the onset of a stroke, which is now the
second leading cause for hospital deaths.
Excerpts...
Q: Has the incidence of strokes risen in the recent past?
A: There has been a serious increase in stroke and resultant
death in Sri Lanka. At present strokes are responsible for the second
largest number of hospital deaths after heart attacks. Although complete
statistics on stroke incidence in Sri Lanka are not available, two
studies carried out suggest that every year more than 1% of our
population develop stroke - that means 200,000 stroke victims annually!
Q: What are the main reasons for this increase?
A: Three major developments are considered the primary causes
for the increase:
1) Lifestyle changes that is associated with urbanisation including
less healthy diets;
2) Higher levels of stress, less exercise and obesity;
3) The rapid ageing of our population, and poor socio-economic status
that continues to be a barrier to access to stroke treatment and
prevention strategies.
That said, poor lifestyle choices could seriously aggravate dangerous
stroke risk factors such as high blood pressure, diabetes and high
cholesterol, especially if strict treatment is not obtained.
Q: You mentioned pressure, diabetes and cholesterol. Can these
non communicable diseases lead to stroke?
|
Recognising a stroke
 Q:What
are the early symptoms of stroke? How do you recognise them? Q:What
are the early symptoms of stroke? How do you recognise them?
A: As the name implies, symptoms of
stroke 'strike' you very suddenly; there is a wide range of
symptoms depending on the area of the brain affected. It is
essential that you are able to recognise the following
warning signs of a stroke:
*Paralysis of one side of the body -
severity could range from a feeling of numbness or an 'anaesthetic'
state to complete paralysis of one side of the body. The
area affected is often, but not limited to, an arm, leg or
half of the face.
*Difficulty in swallowing
*Ataxia - lack of voluntary coordination
of muscle movements (unbalanced, difficulty in walking)
*Loss of balance
*Vertigo - spinning feeling and dizziness
*Slurred speech - inability to vocally
communicate. Recognition is possible and behaviour otherwise
appropriate, yet the victim may not be able to understand
words or speak. If questioned, a response may not be given.
*Sudden, severe headaches with no apparent
cause
*Abnormal eye movements
*Reduction in field of vision from 180 to
90 degrees. Only objects directly in front of the field of
view may be seen, vision of the corners of the surroundings
is reduced when looking straight ahead.
*Loss of vision completely from one eye
*Double vision
*Loss of bladder control
Sometimes a sudden severe headache with no
apparent cause, vomiting and an impaired level of
consciousness can occur, especially in the case of a brain
bleed. |
A: Risk factors for stroke and other non-communicable diseases
such as heart disease and cancer are quite similar. There are two types
of risk factors:
1) Unmodifiable risk factors. These cannot be controlled and include
increasing age, being male in gender, being Asian, and having a family
history of strokes.
2) Modifiable risk factors are treatable or changeable and can be
controlled. They include smoking, high blood pressure, diabetes, atrial
fibrillation (irregular heart rhythm, which predisposes to stroke) and
carotid artery disease (narrowing of the major arteries, which feed the
brain). All these five major risk factors are 'modifiable', which means
if you correct them (by quitting smoking, obtaining treatment for high
blood pressure, diabetes and irregular heart beat) you can prevent a
stroke.
Other modifiable risk factors include obesity, physical inactivity,
high cholesterol levels, certain heart diseases, excessive consumption
of alcohol, use of narcotics, use of contraceptive pills,
post-menopausal hormone replacement, and certain blood diseases.
Q: A common misconception is to confuse a stroke with a heart
attack. Is stroke the cause of heart attacks or vice versa?
A: Stroke is a 'brain attack' and occurs due to either the
clogging of a blood vessel to prevent blood from reaching the brain, or
due to rupture of a blood vessel in or near the brain. A heart attack is
when blood flow to the heart is interrupted causing damage to the heart
muscle.
The symptoms of stroke are very different to the commonly understood
symptoms of heart attack. It is essential to be aware of both and
respond immediately.
Stroke does not cause heart attacks, but due to the similarity of
causative risk factors, a person with a stroke has a higher risk of
developing a heart attack. Heart attacks can give rise to stroke,
especially in the early stages, due to the development of blood clots
within the diseased heart that can become mobile and clog a blood vessel
leading to the brain.
Q: Any other factors to keep in mind?
A: Around a quarter of patients with stroke may experience a
Transient Ischaemic Attack (TIA or mini Stroke). Here the symptoms of
stroke last only for a few minutes and then rapidly resolve. This
condition should be given serious consideration and treatment initiated
immediately as it may be the only warning one may get before developing
a major stroke. Action must be taken early - rush to the nearest base
hospital - not the general practitioner next door. Stroke Units are
available at the hospitals of Colombo (the National Hospital),
Kurunegala, Kalutara, Ragama, Sri Jayewardenepura, Badulla, Ratnapura,
Jaffna and Anuradhapura.
Q: What should NOT be done till help arrives?
A: The brain is very sensitive to the lack of oxygen and
glucose and can only survive between 3 to 5 minutes without them; brain
health is time - so act fast. Do not put food or water into the mouth of
the patient, and do not sit them up as this could increase the risk of
choking. Instead turn them on their side and tilt the head back to open
the airway and prevent them choking on their tongue, especially if they
are unconscious. When the patient attempts to communicate and if they
have difficulty in talking, make suggestions to allow easier
communication. The severity of the stroke can vary, so symptoms may
settle and improve after a while. However, a stroke has still been
experienced - so rush to hospital.
Q: How can stroke be prevented?
A: Even with the most modern treatment facilities, only a
third of patients completely recover from stroke; it is the far better
option to prevent a stroke before it develops. This can be done at two
levels, 'primordial prevention' and 'primary prevention'. In primordial
prevention, lifestyle changes that are commenced early to prevent the
development of modifiable stroke risk factors (which have been outlined
in a previous question above). Primary prevention is for people with
established risk factors who have not yet suffered a stroke; it involves
medication in addition to lifestyle changes to prevent the risk factors
causing a stroke. A third form of prevention, called secondary
prevention, exists for patients who have already suffered a stroke or a
TIA. Here anti-platelet (blood-thinning) treatment is started in
addition to the measures used in primary prevention, to prevent a
further often more severe stroke. It is possible for anyone to assess
their stroke risk using a simple scorecard.
|
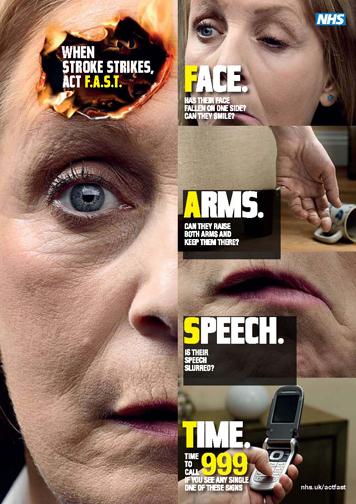
The symptoms
Q. Is there a quick easy way to
recognise these symptoms?
A. The Stroke Association with the
Ministry of Health has put forward a poster for this
purpose. If any of the following 3 checks listed below are
positive, the patient should be taken to the nearest
hospital immediately:
*If the patient is requested to stretch
out both hands in a sleepwalking motion, one hand will drift
downwards, indicating paralysis of muscles. The same process
applies to the legs.
*If asked to bare their teeth in an "ee"
grin (clench the teeth), the mouth is pushed to one side.
This is due to the pull exerted by the muscles that are
properly functioning on the paralyzed muscles, forcing them
towards the healthy side of the face.
*If the patient is spoken to or asked
simple questions, they may be unable to respond. Difficulty
in movement of the tongue may also be observed - if asked to
put their tongue out, this may prove arduous.
However, even they are capable of this,
speech is often impossible; they may not be able to state
their name and address. This is not confusion or a
psychiatric disorder; this is a stroke. Acting fast is vital
again, as the inability to communicate vocally leaves the
patient under conditions of incredibly high stress. |
Q: At the hospital, what is the first line of treatment?
A: All patients with stroke will also be assessed and treated
for possible complications such as infections (of the lungs and the
urinary passage), DVT (clots in the leg veins), pressure ulcers and
depression, which would adversely affect recovery.
Q: What is the next step towards rehabilitating victims?
A: Rehabilitation of a stroke victim requires
multidisciplinary support and is best undertaken in the setting of a
Stroke Unit. A Stroke Unit in a hospital may be a separate section or
part of a ward that cares for stroke patients exclusively. The stroke
unit is composed of: Doctors specially skilled in treating patients,
Nurses who oversee nutrition and care for patients at all times,
Physiotherapists who oversee breathing and chest movements, help in
regaining motion of limbs and breathing., Speech and language therapists
- provide speech exercises, helping communication skills gradually
resurface again. It has been proven that treatment in a Stroke Unit
improves chances of survival and reduces both disability and length of
hospital stay.
Q: The golden rules to follow after a stroke?
A: Avoid foods such as egg yolks, fatty meats, butter and
cream, which are high in fat and cholesterol. Eat moderate amounts of
food and cut down on saturated fat, sugar and salt. Avoid fried food and
take baked or boiled food. Avoid fast food. Eat more fruits, vegetables,
cereals, fish and lean meats.
Q: What about exercise?
A: Guidelines for exercise recommend increased moderate
aerobic physical activity for 150 minutes a week (i.e. 30 minutes a day
for 5 days). There is no limitation to the type of aerobic physical
activity as long as the patient can cope with it safely (especially with
the aim of avoiding falls). |

