
Regional anaesthesia safe for surgeries
by Shanika Sriyananda
Manisha eagerly waited for the feeling of 'labour pains' which her
mother said it would be terrible which can not described what was it.
She proudly announced that she was ready to feel the 'pain'.
 But her swollen legs made her gynaecologist to get her admitted
immediately to a hospital and recommended a C-section as her blood
pressure shot up at the last moment. But her swollen legs made her gynaecologist to get her admitted
immediately to a hospital and recommended a C-section as her blood
pressure shot up at the last moment.
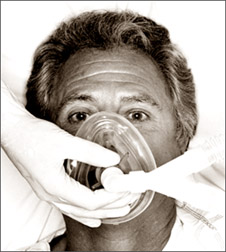
The doctor then decided to give her a regional anaesthesia, whereby
she could watch the medical team get the baby out. Her parents asked the
doctor to give her a general anaesthesia as they believe that regional
anaesthesia may cause more complications later.
The doctor referring to her condition decided on a regional
anaesthesia and now Manisha recalls happily how she heard the baby's
first cry and how the doctors handled the case. And she was even
conscious enough to feel her babies little feet.
"No, there are no such complications related to regional anaesthesia.
It is more safer than the general when in an emergency to perform
surgery, especially the C-sections", Consultant Anaesthetist of the
National Hospital Colombo Dr. Ms. Kumuduni Ranatunge says.
She says that some pregnant mothers ask for regional anaesthesia
because they want to see the baby coming out, so the maternal bond is
immediate and both are awake to get the true feeling.
According to Dr. Ms. Ranatunge, under general anaesthesia the patient
goes to asleep. "But sleeping is not adequate. Standard anaesthesia is a
combination of three requirements the patient is unconscious, adequately
pain re-lived and muscles are relaxed". she adds.
She says that muscle relaxation depends on the condition and
sometimes the patients do not get paralysed the muscles and they are
breathing on their own. "But with anaesthesia there should always be an
anaelgicia, which means pain relief, as well. If you just give one drug
to make the patient only to become unconscious but when you perform the
surgery though the patient may not realise while the surgery is on he or
she could feel the pain.
So, when the patient is still with the pain even though he is
unconscious he will start secreting some hormones, which can bring bad
effects to the body. So, while he is asleep he will have high blood
pressure, very high pulse rate and may sweat. But when he or she wakes
up the patient won't realised it. That is bad for the body", she points
out.
Dr. Ranatunge says that the post operative recovery patients, who
suffered pain during surgery might have problems and during the surgery,
pressure, may shoot up. She says that this condition will give bad
effects on the vital organs like brain, kidneys and heart.
Because, if the patient, is already a hypertension patient, pressure
may go up during the surgery and due to this the patient may get a heart
attack or suffer brain haemorrhage. So balanced anaesthesia is very
important. Responsibility of the anaesthetist is to give a balanced
anaesthesia", she says.
The regional anaesthesia also known as spinal or epidural is injected
to a particular area of the body. Here, according to the wish of the
patient he can be sedated or kept awake. But only the area which needs
anaesthesia will be anaesthetized. According to Dr. Ranatunge, there are
some requirements to fulfil before anaesthetizing a patient.
"The patient should be examined by an anaesthetist to see whether
there could be any problems with the patient which might complicate the
surgery. So, the problems should be ruled out. If the patient has any
problem with the drugs, this should be checked by going through the
patients' history of any reaction to anaesthesia. This is very
important".
"Patients have fast before anaesthesia, especially before a general
anaesthesia. The period is six hours for solid meals and milk. For clear
fluids, like water and plain tea, it is four hours. You should not take
anything within that time period. Because of the risk of gastric
aspiration is there.
Aspiration of stomach contains will pass into the lungs during the
anaesthesia because the patient is unconscious and the muscles in the
throat and larynx are relaxed.
When the stomach is full it can aspirate into the lungs. This
condition is called aspiration numalitist, which has a very high death
rate, because the patient is aspirating solid particles into the lungs"
she explained.
Dr. Ranatunge says that this is the very serious condition during the
pregnancy. A pregnant mother should fast for six hours before undergoing
the surgery. But there are situation where you have to do C-section in
an emergency, when the foetus is not doing well and they need to take
the baby out. In a such a situation you have to make sure that the
stomach is empty.
"Here, the regional anaesthesia is very much preferred and the
patient needs to fast for six hours. As the pregnant mother, in an
emergency, can not fast for six hours, it is safer to give regional
anaesthesia.
On the other hand, the patients stomach is pushed up and with enlarge
abdomen and as the risk of aspiration is high, it is always safer
whenever possible to give a regional anaesthesia, especially when
performing a C-section.
This is mostly safer when there is no contra-indications like spinal
cord problems, deformity in the spine and infections. We have to get the
patient's consent as well. If there is a risk they should be explained",
she adds.
[email protected]
Yoga may help treat depression, anxiety disorders
 Yoga's postures, controlled breathing and meditation may work
together to help ease brains plagued by anxiety or depression, a new
study shows. Yoga's postures, controlled breathing and meditation may work
together to help ease brains plagued by anxiety or depression, a new
study shows.
Brain scans of yoga practitioners showed a healthy boost in levels of
the neurotransmitter gamma-aminobutyric (GABA) immediately after a
one-hour yoga session. Low brain levels of GABA are associated with
anxiety and depression, the researchers said.
"I am quite sure that this is the first study that's shown that
there's a real, measurable change in a major neurotransmitter with a
behavioral intervention such as yoga," said lead researcher Dr. Chris
Streeter, assistant professor of psychiatry and neurology at the Boston
University School of Medicine.
She believes yoga could prove a useful tool to help people battling
depression and anxiety disorders. "We're not advocating that they chuck
their medication, but I would advise that they could use it as an
adjunct and see how they are doing," Streeter said. Her team published
its findings in the May issue of the Journal of Alternative and
Complementary Medicine.
In the study, the Boston researchers used high-tech magnetic
resonance spectroscopic imaging to gauge levels of GABA in the brains of
eight long-time yoga practitioners and 11 non-practitioners. The
participants were healthy, and none was diagnosed with a major
psychiatric condition.
Brain scans were taken before the beginning of the experiment. Then,
the yoga group was asked to engage in the meditative practice for 60
minutes, while the non-yoga group simply read. The researchers then
re-scanned each participant's brain, looking specifically at GABA
levels.
"We showed a 27 per cent increase in the brain GABA levels of those
doing yoga - a really significant increase," Streeter said. No such
change was noted in the non-practitioners who had just read.
She said the style or school of yoga practiced didn't seem to matter.
"We had hatha, ashtanga, bikram, vinyasa, and kripalu" practitioners
included in the yoga group, Streeter said, "and many had been trained in
several different schools." According to Streeter, "this all gives us
one of the mechanisms by which yoga may be having a beneficial effect.
There could be other mechanisms." But another expert pointed to what he
considered flaws in the research.
Zindel Segal, chairman of psychotherapy and a professor of psychology
and psychiatry at the University of Toronto, has for years studied the
use of behavioral interventions to alleviate psychological woes.
He said the Boston researchers were to be commended for using brain
scan imaging technologies to investigate the effectiveness of these
techniques. But he questioned why the yoga group was simply compared to
a sedentary reading group and not to another movement-based group.
"Exercise itself may have some effects on GABA, so I think in this
study, you'd really want that comparison," he said. Including such a
control group would make it clear that it was yoga and not just an hour
of physical exertion that was responsible for the brain changes.
He also pointed out that all of the people in the study were mentally
healthy, and clinical depression and anxiety disorders involve more than
the "daily fluctuations in stress and tension" that healthy individuals
are prone to.
"We know that yoga can have a profound effect" on smoothing out
life's daily ups and downs, Segal said. "But so does working out on a
Stairmaster for an hour." Segal also questioned the role of GABA in
depression.
While it may play a role in anxiety disorders, "GABA is not one of
the main neurotransmitters that seems to be a part of the depression
story," he said. Other neurochemicals - most notably serotonin - play
much bigger roles in the disorder, he said.
None of this means that the study's findings are without merit, Segal
said. "In fact," he said, "we have a program called 'mindfulness-based
cognitive therapy,' where we do use yoga, as well as mindfulness
meditation," as therapeutic tools. Streeter's findings "suggest the need
for more study of these practices," he said.
Streeter agreed that her study is probably just a beginning.
"I think what's important about this study is that it shows that by
using really cutting-edge neuroimaging technology, we can measure real
changes in the brain with behavioral interventions - changes that are
similar to those that we see with pharmacologic treatments," she said.
Would other mind-body practices - Tai Chi, for example - produce
similar effects? "I think that's very possible," Streeter said. "I
suspect that all roads lead up the mountain.
HealthDay News
Risks during pregnancy
by Dr.B.G.A.Vidyatilake, Consultant, Obstetrician
and Gynaecologist
 Pregnancy and childbirth are biological acts necessary for the
propagation of human race. Hence most people believe that they should
occur normally and without complications. Pregnancy and childbirth are biological acts necessary for the
propagation of human race. Hence most people believe that they should
occur normally and without complications.
Whenever a disaster occurs in pregnancy or childbirth there is lot of
commotion and often accusations of negligence against the healthcare
personnel involved.
Is it unnatural for a pregnancy which was normal throughout, to end
up in a complication or even a disaster. Every experienced obstetrician
can quote many such examples. A pregnant mother can become seriously ill
due to severe hypertension, liver or kidney disease or premature
separation of the placenta (afterbirth). Mother may have to undergo a
caesarean section due to the baby developing distress.
Her womb may rupture due to obstructed label, she can have profuse
bleeding after delivering the baby or the womb can turn inside out
(acute inversion). These are grave risks faced by a mother in labour and
can come without warning. Infection can creep into the womb and she can
become seriously ill. In the pre-antibiotic era, a large number of
maternal deaths was due to infection.
These words of the WHO regarding the risks of pregnancy and
childbirth should be an eyeopener. "What is the greatest threat to a
woman's life in developing countries? Complications of pregnancy and
childbirth".
The worst complication associated with pregnancy and childbirth is
maternal death. According to the WHO, about 585000 women die annually
throughout the world due to complications of pregnancy and childbirth.
It means one maternal death per minute, somewhere in the world.
In developing countries 24% of maternal deaths occur in pregnancy,
16% in labour and 60% after the childbirth. It is clear that the risks
of pregnancy continue even after childbirth.
It is not always possible to predict the complications of pregnancy
and childbirth. Identification of high risk pregnancy is the
responsibility of the doctors and maternity healthcare workers. Some of
these risks can be identified on the first clinic visit (short stature,
previous caesarian section, hypertension, diabetes, etc). New risks may
arise in pregnancy and could be identified in subsequent visits. However
majority of complications in pregnancy and labour arise without warning.
Therefore it is prudent to consider that every pregnancy faces risks
and should receive quality care in the antenatal period, during labour
and after childbirth.
How can a woman prepare herself to face the risks of pregnancy and
childbirth?
1. Awareness of risk situations.
2. Regular antenatal clinic attendance.
3. Strict adherence to medical advice.
4. Preparing for childbirth in hospital.
5. Proper management of postpartum period.
6. Avoiding unwanted pregnancy and not seeking unsafe abortions. |
