|

Kidney disease is preventable
By Carol Aloysius
The rising number of patients with chronic kidney problems as well as
those affected by chronic kidney disease of unknown origins (CKdu) has
become a serious health issue in our country. Since the largest number
of patients kidney have been reported from the North Central Provinces,
the Sunday Observer spoke to Consultant Nephrologist Dr Chintana
Galahitiyawa of the Anuradhapura Teaching Hospital to get a better
insight into the causes of this widely prevalent disease, how it could
be prevented, the treatment procedures, as well as the immediate needs
of the hospital.
 ExcerptsÖ ExcerptsÖ
Question: What causes kidney disease?
Answer: Kidney diseases are mainly of two types.
1. Acute (new onset disease of days to weeks which usually be cured
if diagnosed in time and properly treated). Causes include infections
(ex-Leptospirosis and severe infections), Low blood pressure of any
cause.
2. Chronic (long standing slowly progressing kidney damage which
usually is irreversible) causes Ė ex-long standing Diabetes, High blood
pressure
3. Chronic kidney disease of unknown origin (CKDu) is the term used
for north central province kidney disease which is classified as
interstitial nephritis histologically.
Q: Are there different types of kidney disease - e.g. stage
one, stage two and end stage?
A: Chronic kidney disease is divided in to five stages
according to EGFR (Estimated Glomerular Filtration Rate) Normal EGFR 90
to 125
Stage 1 >90 with Asymptomatic urinary abnormalities
Stage 2 - 60 to 89
Stage 3 - 30 to 59
Stage 4 - 15 to 29
Stage 5 <15
End stage renal disease is generally defined as an EGFR of <5
Q: How prevalent is it in Sri Lanka?
A: No recent studies have been done in Sri Lanka to determine the
prevalence.
Q: What are the symptoms?
A: No specific symptoms and the majority are asymptomatic till
they reach advanced stages. Common symptoms include general weakness,
loss of appetite, swelling of the body, body itch and shortness of
breath.
Q: Can they be detected early before going on to stage 11?
A: Yes, in some fortunate patients diagnosed early in routine
medical checkups. At the moment many early stage patients are detected
in the North Central Province (NCP) in the community based screening
programs.
Q: Is it hereditary? Can a parent pass it on to a child?
A: There are rare hereditary kidney diseases. Ex-Alportís
disease, Familial FSGS
Q: Who are the most vulnerable groups to get this?
A: NCP kidney disease is commonly seen among the farming
community.
It usually affects the adults and rare among teenagers.
Q: How can it be prevented?
A: Current belief is that NCP kidney disease is caused by the
toxins contained in agrochemicals and fertiliser such as Arsenic and
Cadmium. Long term exposure to these toxins and accumulation of these in
the kidneys over years cause progressive kidney damage. Minimising
exposure with safe handling of agrochemicals and consumption of safe
water might prevent this disease.
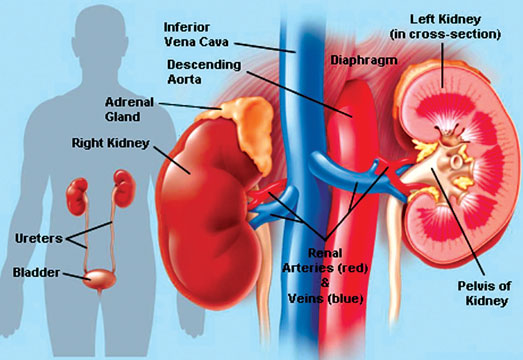
Q: What are the adverse impacts of kidney disease on the body?
A: Kidney is the principal metabolic regulatory organ of the
body. Kidney failure cause metabolic derangement (electrolyte imbalances
such as high potassium and phosphate. Calcium levels will drop.)
Patients become anaemic (low haemoglobin).
They also fail to maintain water balance of the body and patients
urine output drops and develop swelling of the body. Other impacts
include failure to maintain acid-base balance and acidity of blood goes
up. Blood pressure also usually rises and patients tend to develop
coronary artery disease (heart attacks.)
Q: Do they last a lifetime or are they temporary?
A: To treat the above problems, we need to replace the
functions of the kidneys artificially. This is called renal replacement
therapy, such as dialysis or renal transplant. Unless the patient gets
renal replacement therapy, the adverse effects will gradually get worse
and become life threatening.
Q: Does having a kidney stone make you vulnerable to the
disease?
A: There is no evidence to say that they are more vulnerable
to develop CKD-u. But patients with stones are more prone to develop
kidney infections and they can obstruct the urine drainage.
These can subsequently cause chronic kidney disease.
Q: What role do NCDs such as diabetes, hypertension and
cholesterol play as contributory factors?
A: Long standing poorly controlled diabetes and/or
hypertension can cause chronic kidney disease. Diabetes is the commonest
cause for CKD worldwide. Therefore, these can aggravate the severity and
expedite the development of ESRD in NCP kidney disease patients.
 Q: Are there any new breakthroughs in treatment worldwide and
in Sri Lanka? Q: Are there any new breakthroughs in treatment worldwide and
in Sri Lanka?
A: Haemodialysis and renal transplant are the only treatments
available for ESRD.
The advancement of immuno-suppressive therapy during the past decade
has markedly improved the success in renal transplants and their life
span. New dialysis regimens and new equipment have improved the
effectiveness and patients quality of life.
Q: Are there separate wards for patients with kidney problems?
A: There are separate Nephrology wards, at Maligawatte in
Colombo, Sri Jayewardenepura Hospital and Anuradhapura hospital.
Q: How is kidney disease treated? With Drugs? Surgery?
Dialysis?
A: Treatment depends on the CKD stage.
Stage 1 to 5 patients are treated with drugs only.
When they reach End stage, they need to have renal replacement
therapy to live.
Usual initial step is starting regular dialysis.
Dialysis is of two types.
1.Hemo-dialysis - cleaning of patientsí blood and remove excess water
through a complex machine and return back to patients over a short
period of 2.5 to 4 hours twice or thrice a week.
2.Peritoneal dialysis - removes patientsí toxins and excess water by
a special fluid instilled into the peritoneal cavity through a catheter
inserted into the abdominal wall. Itís a continuous procedure and the
fluid instilled in the abdomen is periodically exchanged. Itís done
daily and gives more freedom to the patient.
Unfortunately this is less popular in Sri Lanka. Patients who are
medically fit to have surgery and who have a matching donor are offered
renal transplantation.
Q: How do babies get kidney disease?
A: Causes are different from adults.
Congenital causes are the main factors causing CKD in babies.
Q: Is there a separate ward for them?
A: Paediatric nephrology is a developing field in Sri Lanka.
At the moment they are treated in the paediatric wards and there
arenít any paediatric nephrology wards. But, adults have separate
Nephrology wards. At Colombo Maligawatte, Sri Jayewardenepura and
Anuradhapura hospitals have dedicated adult wards.
Q: What role does diet play?
A: Diet is an important factor in management of kidney
disease. Patients should get adequate nutrition and at the same time,
should avoid certain items that contain harmful substances such as
potassium and phosphates.
Further patients should limit their fluid intake to recommended
amounts when they reach ESRD and on RRT.
Q: When does one need dialysis?
A: When a CKD patient reaches ESRD and when they have
medically uncontrolled metabolic derangements leading to poor quality of
life or toxin levels reaching life threatening quantities.
Q: What is dialysis?
A: Hemo-dialysis- cleaning of patientsí blood and remove
excess water through a complex machine and return to patients over a
short period of 2.5 to 4 hours twice or thrice a week. The hemo dialysis
machine has a part resembling an artificial kidney.
It has a semipermeable membrane which separates patientís blood and
special dialysate fluid flowing on opposite directions.
During this procedure toxins are exchanged into dialysate fluid along
with excess water.
Q: What is CKDu which is now spreading in the North Central
province?
A: Itís a slowly progressive chronic kidney disease which is
mainly seen in north central province and some parts of Uva province.
It mainly affects the middle aged and adult population.
Likely causes are toxins contained in agrochemicals and fertiliser
such as arsenic and cadmium.
Classical areas observed are areas which have the combination of hard
water and high agrochemical/fertiliser usage.
This kidney disease is irreversible and no effective treatment
available to date.
Q: As a Teaching hospital serving over a thousand patients,
does your hospital have adequate facilities to meet the increased number
of kidney patients?
A: At the moment we have adequate infrastructure at
Anuradhapura unit and we will be getting more medical and nursing staff
towards the latter part of this year.
The Minister of health is closely liaising with the NCP renal unit to
fulfill these requirements.
As the number of patients increase day by day the current facilities
need to be improved with time and the plan is to improve the facilities
in peripheral units such as Padaviya, Kebithigollewa and Medawachchiya.
The first satellite dialysis unit will be opened soon at Padaviya.
Q: Your message to the public on preventing kidney disease?
A: As the cause in not clear at the moment for the CKDu, it is
better to take all the precautions to avoid all potential causes such
as;
1. Clean water (bottled, filtered)
2. Safe handling of agrochemicals and fertiliser
3. Minimise the adding of agrochemicals and fertiliser to the
environment
4. Basic screening for hypertension, diabetes and proteinuria
5. Screening for kidney impairment for early diagnosis especially for
relatives of diagnosed patients and people from the same village.
Fatty liver: Is it a scourge of our times?
By Dr. Chandika Liyanage
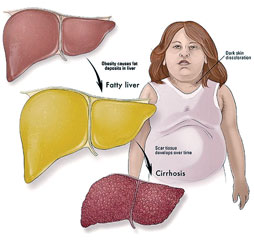
Fatty liver in lay terms can be simply defined as infiltration of the
liver tissue with fat. In scientific terms this means abnormal retention
of triglyceride vacuoles in the hepatocytes or the cells of the liver.
Worldwide the incidence of fatty liver disease is on the rise. The
incidence of fatty liver can range from about 10 to 25 percent. However,
in the United States the incidence of fatty liver disease is about 33
percent. Alarmingly the incidence of fatty liver disease in Sri Lanka is
significantly high.
At the Ragama health study, which was a population-based study
looking at the prevalence of fatty liver disease, showed that 30 percent
of the population had fatty liver disease.
This is further confirmed by our experience at the North Colombo
transplant service where majority of the transplanted patients were
cryptogenic cirrhosis (non alcoholic) patients. Further, as
hepatobiliary surgeons undertaking laparoscopic gallbladder surgery, we
see many patients who have fat infiltrated livers. Majority of these
patients are females. This leaves us with an enormous health problem
threatening our population. Interestingly more than 60 percent of these
patients can have this condition reversed if they opt for a life style
change.
The causes for Fatty liver disease could be alcohol or non-alcoholic.
This is the basis for identifying the two conditions alcoholic fatty
liver disease and non-alcoholic fatty liver disease (NAFLD). The causes
for NAFLD include mainly obesity, which may be associated with insulin
resistance and other metabolic problems. It could be a part of the
metabolic syndrome, which is coined by obesity, diabetes, hypertension
and high lipids. In addition nutritional problems and drugs and toxins
also can result in this disease process.
Transplant
Unfortunately we see many females and some males who present with
cirrhosis of liver requiring transplant. When we dig into their history
we hear unfortunate stories of taking drug concoctions and liver toxins
as form of therapy for long periods of time, slowly destroying their
livers.
Accumulation of fat can progress in to inflammation. This is the
danger of fatty liver disease. This state is called Steatohepatitis, and
in non-alcoholics it is called non alcoholic steatohepatitis (NASH). An
alcohol consumption of less than two drinks per day (20g for women and
30g for men) will be a criterion to include them in to the NASH group.
When there is extensive inflammation and high degree of steaotosis, it
will lead to hepatocyte ballooning and necrosis with progression to
fibrosis.
This will eventually progress to the condition called cirrhosis.
Though the transformation of alcoholic steaotohepatitis to cirrhosis is
clear, the trigger for NASH to progress to cirrhosis is not very clear.
Most of these patients are diagnosed by elevated liver enzymes or due
to liver enlargement and incidentally on ultra sound scan findings.
Generally liver function tests, vial hepatitis serology and imaging
studies, mainly an abdominal ultra sound will help to diagnose this
condition. Though not widely practiced, the confirmation is by a liver
biopsy.
Though much research has been done on this subject there are no clear
answers on treating this condition. Majority of fatty liver disease
patients can reverse the condition by life style modification. The
cardinal step is to avoid the causative factor. If it is alcohol it
should be stopped. All hepato toxins should be avoided. High energy
yielding refined carbohydrate and fat consumption should be minimised to
cut down on the surplus of calories. Exercise helps in improving insulin
resistance and to reduce excess body weight. Up-to-date the only
un-debated form of remedy for fatty liver disease is to lose10 percent
of existing body weight.
Weight
It is important to have good glycaemic control and to achieve ideal
body weight for your corresponding height. Patients should seek
treatment for diabetes and hyperlipidaemias as early as possible and
should screen themselves for this condition, as the prevalence is quite
high in our population.
Alarmingly we now see this condition in the young adult population as
well. When fatty liver sets in early in life there is a high probability
that they will develop liver dysfunction later in life. This will mean
people will require liver transplants unless this condition is taken
seriously. The fact that it is reversible for most is encouraging.
However the effort from the affected is still very discouraging.
(The writer is Consultant Surgeon and Senior Lecturer in Surgery,
North Colombo Teaching Hospital and North Colombo Liver Transplantation
Service). |


