|

World Stroke Day is on October 29:
Prevent, minimise stroke risks with timely treatment
By Carol Aloysius
Stroke continues to be one of the leading disabling diseases and
cause of death in Sri Lanka and worldwide.
Recent studies in Colombo and Gampaha districts have shown that
around one percent of the population develop stroke every year. The
numbers could be higher as there are no national statistics. A worrying
fact is that stroke once perceived to be a disease that affects mostly
elderly persons over 70 years of age, is now seen among younger people
in their late fifties and early sixties. Modifiable and non modifiable
risk factors have contributed to this, says a leading authority on the
subject, who says preventing the modifiable risk factors can eliminate
the danger of developing stroke, while timely interventions and
treatment can minimise the severity of disabilities that result from a
stroke.

Consultant Neurologist and Secretary National Stroke Association Dr
Harsha Gunasekara spells out some of the Do’s and Don’ts to prevent and
to minimise disabilities from the disease, in this interview on the eve
of World Stroke Day.
Excerpts…
Question: Stroke is one of the leading causes of illness and
death worldwide and in Sri Lanka. Compared to the incidence about a
decade ago, is there a significant increase? If so why?
Answer: Stroke is the third leading cause of death and the
leading cause of disability worldwide. In Sri Lanka, stroke has taken
the second or the third place for hospital deaths. However, national
statistics on stroke incidence are not available to date in Sri Lanka.
Two community based studies done in Colombo and Gampaha districts
however, show that around one percent of the population develop stroke
annually.
Q. Is it because we are a developing country, or is it the
same in developed countries in the west? What is the cause of the
difference?
A. There is a definite increasing trend in the stroke
incidence and mortality in the developing countries such as Sri Lanka.
In developed countries, the incidence of stroke is declining, largely
due to efforts to lower blood pressure and reduce smoking.
However, the overall rate of stroke remains high due to the aging of
the population.
Q. What are the main reasons for stroke? Stress? Ageing?
Modern life styles? Poverty?
A. The three major causes for this in developing countries
such as ours include change in lifestyle associated with urbanisation,
increase in the ageing population and poor socio-economic status which
hinders successful strategies for prevention and treatment of stroke.
Q. Are they similar to the factors that have led to a rise in
other non communicable diseases (NCDs)?
A. There is considerable overlap among the risk factors for
stroke and other NCDs (heart disease and cancer), and they are more or
less same for heart disease and stroke.
Risk factors
The five major risk factors for stroke are smoking, high blood
pressure, diabetes, atrial fibrillation (irregular heart rhythm which
predisposes to stroke) and Carotid artery disease (narrowing of the
major arteries which feed the brain).
All these five major risk factors are modifiable, which means that if
you correct them (for example quitting smoking, treating high blood
pressure, diabetes and irregular heart beat) you can prevent a stroke.
The other modifiable risk factors include obesity, physical
inactivity, high blood cholesterol levels, some heart diseases, use of
contraceptive pill and post-menopausal hormone replacement, diseases
which predisposes to abnormal blood clotting, excessive alcohol
consumption, and narcotic drug use.
The non-modifiable risk factors include advanced age, male gender,
and family member with stroke. Those with Asian and afro-Caribbean
ethnicity and low birth weight are also at risk.
Q. Is stroke the cause of heart attacks or vice versa?
A. Stroke is not a cause of heart attacks but due to the
similarity of causative risk factors, a person with a stroke has a
higher risk of developing a heart attack. On the contrary, heart attacks
can give rise to stroke, especially in the early stages due to the
development of blood clots within the damaged heart.
Q. When a person gets a stroke how soon should he or she be
taken to hospital to prevent complications?
A. Most of us are aware that a person with symptoms of a heart attack
should be taken to the nearest hospital immediately. The practice should
be exactly the same after a stroke.
Heart attacks occur due to blockage of a blood vessel feeding the
heart muscle. Similarly, over 85 percent of stroke occur due to blockage
of a blood vessel feeding the brain (the rest due to ruptured blood
vessel causing a brain bleed).
Therefore stroke is a “brain attack”. A person with symptoms of a
suspected stroke should be taken to the nearest hospital immediately.
There are two main reasons for this. Firstly, to perform a CT scan to
rule out or confirm a brain bleed and secondly to initiate treatment
without delay.
Symptoms
Q. What are the early symptoms? How do you recognise them if a
family member develops them at home?
A. As the name implies, symptoms of stroke “strike” you
suddenly.
There is a wide range of symptoms depending on the area of the brain
affected and the common ones are numbness or weakness of one side of the
body or one limb alone, disturbance of speech, impaired vision in one
eye or double vision, impaired balance and co-ordination and impaired
swallowing and bladder control.
Sometimes headache, vomiting and impaired level of consciousness can
occur especially in the case of a brain bleed.
Since remembering all these symptoms is difficult, Stroke
Organisations have put forward a simple test called FAST – Face, Arm,
Speech, Time which is explained in the diagram. If any of the three
checks are positive, the patient should be taken to the nearest hospital
immediately.
Around a quarter of patients with stroke may experience a Transient
Ischaemic Attack (TIA or mini stroke). Here the symptoms of stroke last
only for a few minutes and then rapidly resolve. This condition should
be given serious consideration and treatment initiated as it may be the
only warning one may get before developing a major stroke.
Treatment
Q. What is the first line of treatment?
A. Doctors will first assess the patient to confirm a stroke
and determine the risk factors, then do investigations including a CT
scan. Initial treatment involves monitoring and controlling the blood
pressure (which should not be too high or too low in the early stages
after a stroke), blood glucose level, oxygen level, and if needed
measures to reduce brain swelling.
Once a brain bleed is ruled out, blood thinning (anti-platelet)
treatment is initiated. Patients will also be given cholesterol lowering
drugs.
If the patient is brought to the hospital and a brain bleed is ruled
out within three hours, clot buster treatment is given in a few
hospitals where it’s available.
All patients with stroke should also be assessed and treated for
possible complications such as infections (of the lungs and the urinary
passage), DVT (clots in the leg veins), pressure ulcers and depression.
Stroke patients should be managed with the aim of preventing these
complications which would otherwise adversely affect recovery from
stroke.
Q. Thereafter what is the next step towards rehabilitating
victims?
A. Rehabilitation of a stroke victim requires multidisciplinary
support and is best - undertaken in the setting of a stroke unit. A
Stroke Unit is a hospital unit (may be separate or part of a ward) that
cares for stroke patients exclusively or almost exclusively, with
specially trained staff and a multidisciplinary approach to treatment
and care. The multidisciplinary team consists of doctors, nurses,
physiotherapists, occupational therapists, speech and language
therapists, psychologists/counsellors and a social worker.
It has been proven that treatment in a stroke unit improves chances
of survival and reduces both disability and length of hospital stay.
Q. After a stroke, are there any dietary guidelines?
A. Dietary guidelines are not specific for stroke victims but
should be followed by all to prevent a first or a recurrent stroke and
other NCDs.
The diet should be rich in fruits and vegetables and low-fat dairy
products and reduced saturated and total fat, sugar and salt. Cessation
of smoking and limitation of alcohol intake are essential.
Q. What about exercise? Can a stroke victim cycle, swim, walk,
climb stairs, carry weights/play tennis?
A. Guidelines for exercise recommend increased moderate
aerobic physical activity for 150 minutes a week (i.e. 30 minutes a day
for five days).
There is no limitation of the type of aerobic physical activity as
long as the patient can cope with it safely (especially with the aim of
avoiding falls).
Q. Is there a limit to such exercises? Do they have to be
under medical supervision?
A. Supervision and guidance by a physiotherapist or carer may
be needed in the initial period. In the presence of heart or lung
disease, close medical supervision may be required.
Q. Once a stroke victim, are you always a stroke victim?
A. Not necessarily. On average after a stroke, one-third of
patients fully recover or will be left with only minor disability.
Another third will be significantly disabled for life. One-third of
patients will die, either directly as result of the stroke or due to one
of its complications.
Duration of recovery is variable and depends on the severity of
stroke, age of the patient, presence of complications and the setting of
post-stroke care. Majority of patients who do recover usually regain
physical functions and activities of daily living over a period of
approximately two - four weeks.
Stroke victims carry a higher risk of developing a second stroke,
irrespective of their level of recovery.
Approximately one quarter of strokes occur in patients who have
already suffered a stroke.
Therefore, patients should strictly adhere to the advice given on
lifestyle modifications and the treatment prescribed to prevent another
stroke.
Q. In some countries there are stroke units where patients get
everything they need from treatment to rehabilitation and counselling.
Does the National Hospital have this facility and also any private
hospital? Tell us more about the functions of this unit.
A. The first Stroke Unit in Sri Lanka was set up at the
Institute of Neurology of the National Hospital in 1998 by Consultant
Neurologist Dr Jagath Wijesekera who was also the Founder President of
the National Stroke Association.
Thereafter, stroke units have been established in several provincial
hospitals largely due to the advocacy of the National Stroke Association
and its past presidents together with the initiative taken by the
Ministry of Health.
Some private hospitals too have Stroke Units.
Q. Your message to the public?
A. Avoid all modifiable risk factors such as smoking, drinking
excessive alcohol, and narcotic use.
If you have a non communicable disease like diabetes or hypertension,
take the prescribed medication regularly.
If you are a stroke patient, adhere to the advice given on lifestyle
modifications and treatment prescribed, to avoid another stroke.
World faces looming stroke epidemic, health experts warn
The world is facing a “looming stroke epidemic” experts have warned
after a global study revealed a huge leap in the numbers of younger
people suffering from a condition previously associated with old age.
A third of all strokes now occur in 20 to 64-year-olds, according to
the Global and Regional Burden of Stroke study.
Incidence in this age group has increased by a “startling” 25 percent
in just 20 years said the authors of the report, published in The
Lancet.
In the under 20s, more than 83,000 strokes are recorded every year -
one in every 200 cases.
A second report, published in The Lancet Global Health, shows that,
while overall death rates were down, the number of people dying from
stroke was ten times higher in low and middle income countries compared
to rich countries. The authors predict that the amount of disability,
illness and premature death caused by stroke will more than double
worldwide by 2030.
In the UK, there are around 152,000 strokes every year, and the new
findings reveal that the poorest areas of the country had a three times
higher death rate than the richest.
Jon Barrick, chief executive of the Stroke Association, said that the
report revealed “shocking disparity” between rich and poor.
“These new findings lay bare the formidable challenge facing local
health services, not only in the UK, but also in countries around the
world, to tackle a looming stroke epidemic…” he said. “To help close
this health inequality gap, we need more investment in stroke prevention
and research.”
He warned that rising rates of obesity and diabetes could “wipe out”
gains made in reducing stroke mortality in the UK and said that “at
least half of strokes” could be prevented by keeping blood pressure
under control and exercising more.
More than half of the global deaths and the majority of the
disability caused by stroke were a result of haemorrhagic strokes, the
most deadly form, which is mainly caused by high blood pressure and
unhealthy lifestyles.
Commenting on the studies for The Lancet, Maurice Giroud, Agnes
Jacquin, and Yannick Béjot from the University of Burgundy’s department
of neurology said: “Despite some improvements in stroke prevention and
management in high-income countries, the growth and ageing of the global
population is leading to a rise in the number of young and old patients
with stroke.
“Urgent preventive measures and acute stroke care should be promoted
in low-income and middle-income countries, and the provision of chronic
stroke care should be developed worldwide.”
The Independent
Protecting the brain starts at the synapse
New research by scientists at San Francisco shows that one of the
brain's fundamental self-protection mechanisms depends on coordinated,
finely calibrated teamwork among neurons and non-neural cells known as
glial cells, which until fairly recently were thought to be mere support
cells for neurons.
The study, which has implications for understanding neurodegenerative
diseases, stroke, and other nervous system disorders, adds to a growing
body of evidence that glial cells are integral to brain function.
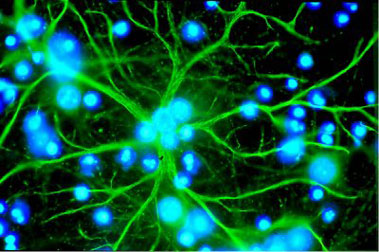 Because this mechanism is localised at synapses, the sites where
communication between neurons takes place, said Marta Margeta, assistant
professor of pathology and senior author of the new study, it ensures
that protective measures will only be taken when and where they're most
needed. Because this mechanism is localised at synapses, the sites where
communication between neurons takes place, said Marta Margeta, assistant
professor of pathology and senior author of the new study, it ensures
that protective measures will only be taken when and where they're most
needed.
“The President needs more bodyguards than a Congressman, and with
this system you can have your cake and eat it too: protection when you
need it, without having to have it everywhere.”
The brain is the body's hardest-working organ, consuming as much as
25 percent of our overall energy. This metabolic demand makes brain
cells particularly vulnerable to damage from oxidative stress, in which
reactive oxygen species (ROS), sometimes called free radicals, exert
toxic effects on cellular components.
ROS damage to neurons has been implicated in Alzheimer's disease,
Parkinson's disease, and other neurodegenerative conditions.
The brain can also be severely damaged when disease or injury -
especially stroke - causes neurons to repetitively fire, flooding brain
tissue with toxic levels of the excitatory neurotransmitter glutamate, a
condition known as excitotoxicity.
To counteract the potential damage arising from ROS, excitotoxicity,
and other dangers, animals including humans have evolved sophisticated
physiological defenses such as the Nrf2 pathway, a molecular network
that triggers the expression of a suite of protective genes when
cellular function is under threat.
It is Neuroscience 101 that neurons pass on electrochemical messages
at communication sites called synapses, but it is less well appreciated
that the vast majority of synapses are “tripartite,” consisting not just
of a neuron sending a message and one receiving it, but also, nestled
alongside each synapse, a star-shaped glial cell called an astrocyte.
Experiments in mouse models of Parkinson's disease and amyotrophic
lateral sclerosis (ALS, or Lou Gehrig's disease) have demonstrated that
Nrf2-based neural protection is primarily conferred by astrocytes, but
how neurons might alert astrocytes to stressful conditions is poorly
understood.
When the research team tried to activate the Nrf2 pathway in
predominantly neural or astrocytic cultures by bathing them with a
substance that creates conditions mimicking excitotoxicity, they had
little success, but in mixed cultures the pathway was set in motion.
These experiments demonstrated that both neurons and astrocytes are
necessary for Nrf2 activity.
However, because the treatments affected the cultures globally and
did not precisely target synapses, the researchers next applied
substances that increase the firing of glutamate neurons by acting
solely at synaptic sites.
Again, Nrf2-related activity was observed only when astrocytes were
present in cultures, but significantly, Nrf2 signalling increased in
tandem with neuronal firing, suggesting that neurons calibrate Nrf2
activity in astrocytes to keep pace with neural activity.
This precise calibration remained intact even when there was no
physical contact between neurons and astrocytes in culture, indicating
that neurons secrete some soluble factor that activates Nrf2 in
astrocytes.
When excitatory neurons fire and release glutamate neurotransmitter
into the synapse, the released glutamate can reach nearby astrocytes, so
glutamate seemed a good candidate for the neuronal messenger that
induces Nrf2 activity.
- MNT
|

